Medical professionals, law enforcement and government officials gathered at Stony Brook University this past weekend to have an open and honest dialogue about the growing opioid problem facing the North Shore and the rest of Suffolk County.
The complexity of the problem and how it relates to communities across the county was the topic of the discussion Oct. 1. A common theme among the speakers was opioid addiction should be treated like a legitimate medical crisis and not a moral failing.
Dr. Constantine Ioannou, director of Stony Brook Medical Center’s Adult Inpatient Unit addressed the current opioid crisis in the United States and specifically in Suffolk County during the event.
“This is not the first opioid epidemic in the United States — this is one of many,” Ioannou said. He likened the current state of opioid prescribing and subsequent widespread addiction to a period in the late 1800s when morphine was first developed. He said doctors overprescribed the powerful painkiller and, in turn, opioid dependence skyrocketed.

The director traced the origin of the current crisis back to two events in 1995. Purdue Pharma, a pharmaceutical company, began marketing OxyContin, its version of the powerful opioid oxycodone, to doctors. In addition the American Pain Society, an organization dedicated to advocating for public policies to reduce pain-related issues, named pain as the fifth vital sign. Like the other four — pulse rate, temperature, respiration rate and blood pressure — pain would be monitored in patients from then on. Pain was the only one of those five vital signs that is completely subjective and based on what a patient tells a nurse or doctor, Ioannou said.
Those two events, in accordance with nurse ratings and even payment being tied to patient satisfaction and reduction, created an environment of overprescribing, Ioannou said. He also said training of doctors in pain management needs to be addressed — he graduated from medical school in 1985 with “zero” training in pain management.
“There are states in the United States where there are more prescriptions for opiate pain medications than there are people — this is a staggering number,” Ioannou said.
Jermaine Jones, Ph.D., an assistant professor of clinical neurobiology in the Department of Psychiatry at Columbia University, also spoke and reiterated some of what Ioannou said regarding the United States’ views on pain management.
“I’ve had friends from other countries say that unless you come into the E.R. with an arm missing, you’re not going to get a prescription that you could get here for having a root canal,” Jones said. “We make up about 5 percent of the world’s population yet we consume about 80 percent of the prescription opioid [painkillers].”
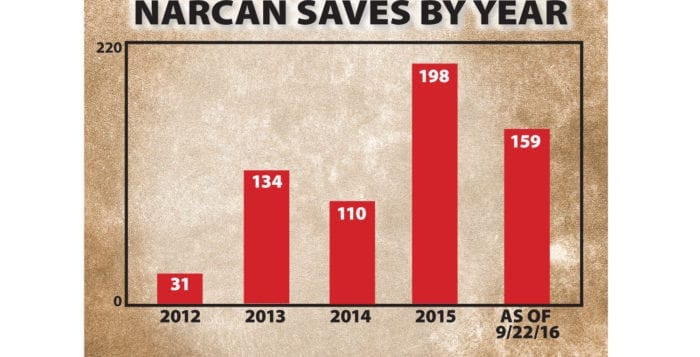
Jones is involved in a study called Risks and Benefits of Overdose Education and Naloxone Prescribing to Heroin Users and spoke about some of his findings. Naloxone, commonly known by the brand name Narcan, is a drug used to reverse opioid overdoses.
“We’re trying to better understand how to tease apart ways to attenuate what people like about opioids,” Jones said of the five-year study, which is currently in its second year.

He said the study was created to monitor people who are administered naloxone and see if it is being used for the correct purposes. One concern in the creation of an overdose reversal drug is that users will be more confident in their ability to combat an overdose and may decide not to call 911 if that day ever comes. Other potential unintended consequences of naloxone, including how to deal with a user who may be irate after being saved from an overdose and is now “dope sick” and without the expensive drug they just bought, are the focus of the study. They are also researching some potential new medications or existing ones that could work in accordance with opioids to reduce pain, while reducing the effects that lead to addiction.
“We know that detox by itself is actually one of the highest risk factors for opioid overdose because you’re tolerance decreases,” Jones said. “So once someone comes out of a detox program they swear they’re never going to touch this stuff again, but relapse is very, very common. So they use again thinking that if they were using two bags before, they can continue using two bags now that they’ve gotten out, but their physiological tolerance has decreased and people overdose as a result.”
Ioannou indicated he’d like to see changes in treatment options for addicts.
“We treat all addiction by the same model,” he said. “You have a five-day detox, 28-day rehab and you have an after care that is all based on 12 steps. That is the model of care in the United States. We need to realize with a complex disease, you need a complex set of interventions.”
Suffolk County Police Department Deputy Sheriff Mike Kern is an expert in recognizing drug users. He called overdoses the most powerful “advertisement” for drug dealers because it is a clear indication of how strong their product is. He echoed sentiments from both doctors about the dangers of overprescribing and to what it can lead.
“Why can a doctor prescribe an OxyContin to a 16-year-old or a 15-year-old who just had a root canal?” Kern asked. “It just doesn’t make any sense.”