By David Dunaief, M.D.
Autoimmune diseases are becoming increasingly common, affecting approximately 23.5 million Americans, with 78 percent of them women. These numbers are expected to continue rising. There are more than 80 conditions with autoimmunity implications (1). These diseases include rheumatoid arthritis (RA), lupus, thyroid (hypo and hyper), psoriasis, multiple sclerosis and inflammatory bowel disease, to mention just a few.

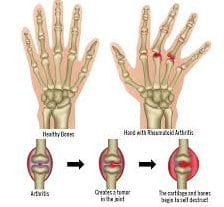
Autoimmune diseases are defined by the immune system inappropriately attacking organs, cells and tissues of the body, causing chronic inflammation. Thus, inflammation is the main consequence of immune system dysfunction, and it is the underlying theme tying these diseases together. Unfortunately, autoimmune diseases tend to cluster (2). In other words, once you have one, you are much more likely to acquire others.
Drug treatments
The mainstay of treatment is immunosuppressives. For example, in RA where there is swelling of joints bilaterally, the typical drug regimen includes methotrexate and TNF (tumor necrosis factor) alpha inhibitors, like Remicade (infliximab). These therapies are thought to help reduce the underlying inflammation by suppressing the immune system and interfering with inflammatory factors, such as TNF-alpha. The disease-modifying antirheumatic drugs (DMARDs) may slow or stop the progression of joint destruction and increase physical functioning. Remicade reduces C-reactive protein (CRP), a biomarker of inflammation.
However, there are several concerning factors with these drugs. First, the side effect profile is substantial. It includes the risk of cancers, opportunistic infections and even death, according to black box warnings (the strongest warning by the FDA) (3). Opportunistic infections include diseases like tuberculosis and invasive fungal infections. It is no surprise that suppressing the immune system would result in increased infection rates. Nor is it surprising that cancer rates would increase, since the immune system helps to fend off malignancies. In fact, a study showed that after 10 years of therapy, the risk of cancer increased by approximately fourfold with the use of immunosuppressives (4).
Second, these drugs were tested and approved using short-term randomized clinical trials, but many patients are put on these therapies for 20 or more years. Remicade’s package insert was approved with approximately two years of data.
So what other methods are available to treat autoimmune diseases? These include medical nutrition therapy using bioactive compounds, which have immunomodulatory (regulation of the immune system) effects on inflammatory factors and on gene expression, and supplementation.
Nutrition and inflammation
Raising the level of beta-cryptoxanthin, a carotenoid bioactive food component, by a modest amount has a substantial impact in preventing RA. In one study, participants drank the equivalent of about one glass of freshly squeezed orange juice a day with a resultant 49 percent risk reduction in the development of RA (5).
While I have not found studies that specifically tested diet in RA treatment, there are dietary studies that have shown anti-inflammatory effects in other diseases, using biomarkers such as CRP and TNF-alpha. In a study that looked at the Mediterranean-type diet in 112 older patients, there was a significant decrease in inflammatory markers, including CRP (6).
In another study, participants showed a substantial reduction in CRP with increased flavonoid levels, an antioxidant, from vegetables and apples. Astaxanthin, a carotenoid found in fish, was shown to significantly reduce a host of inflammatory factors in mice, including TNF-alpha (7).
Vitamin D
Vitamin D is ubiquitous in helping to treat and prevent many chronic diseases — autoimmune diseases are no exception. Vitamin D affects over 200 genes, according to Wellcome Trust Centre for Human Genetics at University of Oxford. In the absence of vitamin D, T-cell response, part of the immune system, becomes dysfunctional and uncontrollable, resulting in an increase in multiple sclerosis (MS) and inflammatory bowel disease — Crohn’s and ulcerative colitis. However, when normal levels of vitamin D are conveyed to the vitamin D receptors, proper T-cell functioning is restored with no subsequent autoimmune disease, at least in animal studies (8).
Interestingly, multiple sclerosis patients are notoriously very low in vitamin D, and it is difficult to raise the levels. There was a small study proclaiming that MS patients may need as much as 50,000 IUs of vitamin D2 weekly, and that it was safe (9). I would check with a neurologist specializing in MS before taking such a high dose.
Fish oil

If you think vitamin D is impressive, fish oil affects as many as 1,040 genes (10). In a randomized clinical study, 1.8 grams of eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) supplementation had anti-inflammatory affects, suppressing cell signals and transcription factors (proteins involved with gene expression) that are pro-inflammatory, such as NFkB.
In RA patients, fish oil helps suppress cartilage degradative enzymes, while also having an anti-inflammatory effect (11). When treating patients with autoimmune disease, I typically suggest about 2 grams of EPA plus DHA to help regulate their immune systems. Don’t take these high doses of fish oil without consulting your doctor, since fish oil may have blood thinning effects.
Probiotic supplements
The gut contains approximately 70 percent of your immune system. Probiotics, by populating the gut with live beneficial microorganisms, have immune-modulating effects that decrease inflammation and thus are appropriate for autoimmune diseases. Lactobacillus salvirus and Bifidobacterium longum infantis are two strains that were shown to have positive effects (12, 13).
In a study with Crohn’s disease patients, Lactobacillus casei and L. bulgaricus reduced the inflammatory factor, TNF-alpha (14). To provide balance, I recommend probiotics with Lactobacillus to my patients, especially with autoimmune diseases that affect the intestines, like Crohn’s and ulcerative colitis.
Fiber
Fiber has been shown to modulate inflammation by reducing biomarkers, such as CRP. In two separate clinical trials, fiber either reduced or prevented high CRP in patients. In one, a randomized clinical trial, 30 grams, or about 1 ounce, of fiber daily from either dietary sources or supplements reduced CRP significantly compared to placebo (15).
In the second trial, which was observational, participants who consumed the highest amount of dietary fiber (greater than 19.5 grams) had reductions in a vast number of inflammatory factors, including CRP, interleukin-1 (IL-1), interleukin-6 (IL-6) and TNF-alpha. (16).
Immune system regulation is complex and involves over a 1,000 genes, as well as many biomarkers. Dysfunction results in inflammation, and potentially autoimmune disease. We know the immune system is highly influenced by bioactive compounds found in high nutrient foods and supplements. Therefore, bioactive compounds may work in tandem with medications and/or may provide the ability to reset the immune system through immunomodulatory effects and thus treat and prevent autoimmune diseases.
References: (1) niaid.nih.gov. (2) J Autoimmun. 2007;29(1):1. (3) epocrates.com. (4) J Rheumatol 1999;26(8):1705-1714. (5) Am J Clin Nutr. 2005 Aug; 82(2):451-455. (6) Am J Clin Nutr. 2009 Jan;89(1):248-256. (7) Chem Biol Interact. 2011 May 20. (8) Prog Biophys Mol Biol. 2006 Sept;92(1):60-64. (9) Am J Clin Nutr. 2007 Sep;86(3):645-651. (10) Am J Clin Nutr. 2009 Aug;90(2):415-424. (11) Drugs. 2003;63(9):845-853. (12) Gut. 2003 Jul;52(7):975-980. (13) Antonie Van Leeuwenhoek 1999 Jul-Nov;76(1-4):279-292. (14) Gut. 2002;51(5):659. (15) Arch Intern Med. 2007;167(5):502-506. (16) Nutr Metab (Lond). 2010 May 13;7:42.
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management.