By Elana Glowatz & Rachel Shapiro
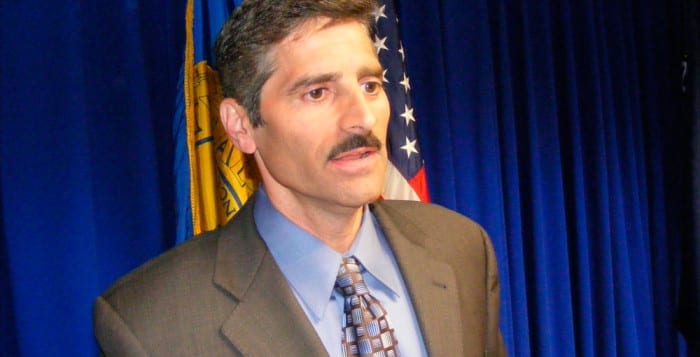
Former County Executive Steve Levy was under no illusions that he would make friends when he took Suffolk’s top office eight years ago.
He stood his ground in long-term battles with the Suffolk County Police Benevolent Association and the Legislature and he says that paid off. When the PBA took out anti-Levy ads after the county executive shuffled police officers around to cut costs, he took it all in stride.
“You’ve got to have the backbone to stand up to that and not wilt,” Levy said in an interview. “Over time you’ll be proven correct, as we were with the highway patrol change and as we were with civilianization.”
PBA second vice president Noel DiGerolamo fired back in a phone interview Tuesday that “the only thing that was proven over time is that Steve Levy was not a person to be trusted or believed, as proven by his departure from the government … and his ongoing legal troubles with the [district attorney].” DiGerolamo was referring to Levy’s return of $4 million in campaign funds as part of an agreement with District Attorney Tom Spota, under which the county executive also agreed not to seek a third term.
Levy, 52, has declined on several occasions to discuss the details of the deal.
Other battles aside, Levy considers county Comptroller Joe Sawicki and Newsday’s editors and reporters to have played a part in trying to tarnish his reputation. In reflecting on his time as county executive, he painted a picture of the comptroller and the newspaper working to embarrass and discredit him.
Control battle with comptroller
One example he gave is Sawicki’s office performing an audit on the request for proposals process to sell the county-owned John J. Foley Skilled Nursing Facility, to determine whether the county had followed procedures correctly. Levy said he was interested in selling the nursing home to save the county money. When the report was completed, Levy said, the comptroller then “conveniently drops it on the table of the Legislature the same day they’re voting” on the sale, in order to sway the legislators to kill it.
But the comptroller told a different story. In an interview with Times Beacon Record Newspapers following Levy’s allegations, Sawicki said Presiding Officer Bill Lindsay (D-Holbrook) and legislators Kate Browning (WF-Shirley) and John Kennedy (R-Nesconset) requested the audit in November 2010, and his office was rushing to complete the report by March 2, 2011, the day of the vote. And according to Christina Capobianco, Sawicki’s chief deputy comptroller, the audit staff was “stonewalled” by the county Health Department and attorney’s office, delaying the process.
‘I think he became extremely paranoid over the years.’ — Joe Sawicki
However, Levy was not convinced. “It’s too cute to just so happen to finish your audit on the same day that the Legislature is voting on this issue,” he said. “If [Sawicki] was concerned about timing he simply could have mentioned this to the Legislature. He never did. … This was an 11th hour surprise to try to kill the deal.”
The Legislature ultimately voted to sell the nursing home, but the buyer, Kenneth Rozenberg, was no longer interested.
Levy said Sawicki had an agenda against him. He pointed to the fact that at the same time the nursing home audit was being performed, Sawicki donated money to the Nursing Home Support Fund for employees who were working to save the facility from closure, and he attended a fundraiser.
According to a New York State Board of Elections financial disclosure report, Sawicki donated $500 to that group on Jan. 10, 2011.
Levy called the act a conflict of interest and said that Sawicki was considering a run for county executive and was buying the support of the nursing home employees’ union. But the comptroller said although others had suggested it to him, he had not planned to run for county executive, and that his office’s audit and his support of keeping the nursing home open were “totally separate.”
Sawicki said his wife is a geriatric nurse at a private nursing home and that the Foley facility had a place in his heart.
“In my mind, helping the employees contribute to their legal fund to fight to stay open and keep their jobs is a lot different than an audit I was doing of the RFP process,” Sawicki said. “I would do it all over again.”
‘It’s too cute to just so happen to finish your audit on the same day that the Legislature is voting on this issue.’ — Steve Levy
In addition to Levy’s claim that Sawicki was trying to cast him in a negative light because of a potential run for county executive, Levy said there was friction because he would not approve some of the comptroller’s hires in order to save money.
Sawicki said Levy would block approval of employees hired within his department’s approved budget. Ultimately, various elected county officials called for legislation that would allow them to approve their own hires if they stayed within their budgets. The legislation passed.
Although Sawicki expressed frustration with the hiring situation, he said he never did anything to give Levy a bad name. “You can’t find anything that I did that exceeded my role as the comptroller,” Sawicki said. “I pride myself on being the chief fiscal watchdog. I like that title.”
The comptroller also said that Levy didn’t like being audited and “I think he became extremely paranoid over the years.”
Levy responded, “If I didn’t want him doing audits I would have been complaining from my first year in office.” He added, “It’s absolutely his role to do audits.”
Financial disclosure
The county executive also took issue with Newsday’s coverage of various subjects, including his financial disclosure forms and wife Colleen West-Levy’s business. In a series of articles beginning in 2010, Newsday investigated Levy’s filing of the state-mandated financial disclosure form.
Throughout some of Newsday’s stories, such as “Disclosure bill would force Levy to report to county,” published June 15, 2010, the reporter stated as a matter of fact that the county form was more thorough than the state form that Levy was filing. This statement was not attributed to any source. In at least one other story, the reporter has also cited unnamed officials for this information.
In the stories, the reporter interviewed political opponents of Levy, who are quoted as saying that the county executive was in violation of county law when he filed state forms instead of county forms.
Levy argued that the reporter left out crucial information, including three expert opinions, one from Mark Davies, that cited Levy’s requirement to file the state form and his compliance with county law.
Davies, former executive director of the Temporary State Commission on Local Government Ethics, has served on several ethics committees, including as co-chair of the Ethics Committee of the American Bar Association’s section of state and local government law. He is also an adviser to the American Law Institute’s Project on Public Integrity and an adjunct professor of law at Fordham Law School.
‘Newsday is proud of its reporters and editors who pursued this story thoroughly and fairly while withstanding repeated criticisms and even personal attacks.’ — Statement from Newsday
He said in a written testimony to the Suffolk County Legislature in September 2010, “Indeed a comparison of the state form and the Suffolk County form reveals that, on the whole, the state form is more extensive than the county form.” He gave examples of disclosure categories the county form does not include, such as offices in political parties and organizations; the nature of a filer’s business; agreements for future employment; assignments and transfers of income and interest to others for less than fair market value; securities held by a corporation for investment when the filer or his or her spouse owns or controls 50 percent or more of the corporation; gifts and reimbursements; and any information on the assets and liabilities of the filer’s dependent children.
The county form also does not ask the filer to list unpaid positions with entities that have no current business or licenses with the county, even if they had immediate past county business or have upcoming county business.
Davies argued that because the county form lacks these categories, it does not comply with state law. He recommended that the county adopt the state form, at least on an interim basis, until the county form is brought into compliance with state law.
In the past year, legislation has been introduced to bring the local form into compliance with New York State law.
Levy said he gave the reporter the information from Davies early on in the reporting to include in the story, but it was not printed.
In Newsday’s story “Levy defends financial disclosures,” published June 9, 2010, a chart compiled by the reporter highlights specific information that is required on the county form and not the state’s — but not vice versa. The chart correctly says the county form requires the filer list bank accounts, including the type of account, the nature of ownership and the name of the bank. The state form does not require this information.
With regard to real estate interests, both forms require disclosure of location, size, general nature, acquisition date, percentage of ownership and range of value of the property. The only difference between the forms is that the county’s requires the filer to name partners and the valuation date. The chart incorrectly states that the state form does not require market value. The form specifically asks for approximate market value.
The chart also incorrectly says that the state form does not ask the filer to list credit card debt. In fact, the filer must list liabilities, but the form provides many exceptions, credit card debt not being one of them. Tim Glynn, an attorney in Setauket concentrating in business law, said a credit card balance should be reported, according to the language of the form. However, if the balance was accrued by purchasing items that were exempted, the filer could leave the debt off the list.
Newsday’s chart correctly says the state form does not require disclosure of government contracts secured through competitive bidding or requests for proposals, while the county form does.
“What [the reporter] would gloss over and not put in is that I was required by law to file a state form instead of a county form,” Levy said. “Newsday tried to make it look like I was forum shopping for a particular form to file because I wanted to hide something. It’s total nonsense.”
Levy is required by state law to file the state form as a sitting member of the Pine Barrens Commission, a state agency. This fact was confirmed by the county Ethics Commission in a 2006 ruling. For his first two years in office, Levy filed both state and county forms. Following the ruling in 2006, he began filing only the state form. Similar to wording in other stories, Newsday describes the ruling in “Levy defends financial disclosures” by saying, “The county ethics commission — whose members were appointed or recommended by Levy — has allowed him to file a state disclosure form since 2006.” Levy argues that the language used makes it appear as if the commission is giving him special treatment when, in fact, it is upholding state law.
Despite this, in 2010 Levy filed county forms from the years he had missed — from 2006 to 2009. In an interview, Levy said he filed the county form for those years because he had nothing to hide.
Times Beacon Record Newspapers sat down with Newsday’s vice president of public affairs, Paul Fleishman, and presented Levy’s claims about Newsday. The paper declined to give responses to each allegation, and instead issued the following statement:
“The facts speak for themselves. Last year, following an investigation by the Suffolk County District Attorney’s office, then-Suffolk County Executive Steve Levy forfeited $4 million of campaign money and announced he would not run for re-election. Newsday is proud of its reporters and editors who pursued this story thoroughly and fairly while withstanding repeated criticisms and even personal attacks. Newsday has a long and respected history of straightforward and courageous investigative reporting on behalf of the people of Long Island, who depend on us to shed light on matters that are important to the public. It is a responsibility to our community that we take very seriously, approach thoughtfully and pursue with the utmost care, integrity and commitment to accuracy. We stand firmly behind our reporting and our coverage.”
Colleen West-Levy
As it probed Levy’s financial disclosure forms, Newsday also questioned the business practices of his wife, Colleen West-Levy. Specifically, Newsday listed companies that had worked with West-Levy’s firms and had also received county funds, seeking to determine if there was a connection between the two. West-Levy’s court reporting and transcription businesses, Enright and Enright Sten-Tel, had a relationship with various companies that contracted with the county, five of which were law firms that Newsday named in the July 8, 2010 article “A question of disclosure.” While the story said that three of those firms had a relationship with West-Levy’s companies before her husband took office, Levy said his wife had worked with all of them before he took office and the work was not the result of political connections.
Levy estimated that of his wife’s roughly 200 clients, only 10 to 15 of them had any connection to the county.
The article also named Stony Brook University Medical Center’s Cody Center and Good Samaritan Hospital, based in West Islip, in the investigation as to whether there could be a connection between the hospitals receiving county funds and West-Levy’s businesses working with the institutions.
A 2005 ruling from the Ethics Commission stated that West-Levy could continue her work with Stony Brook University Medical Center and with any other hospital in the county without posing a conflict of interest.
“To any objective reporter, that 2005 opinion from the county’s Ethics Commission should have ended any thought of this sensationalistic ‘gotcha’ story,” Levy said in a statement.
‘This inaccurate and irresponsible series of articles [goes] to great lengths to insinuate that Colleen built her businesses upon my becoming county executive.’ — Steve Levy
Levy takes issue with the nature of the stories about his wife. The lead of the July 8 story states, “Court reporting firms owned by Suffolk County Executive Steve Levy’s wife, Colleen West, have regularly received work from businesses that have been paid millions of dollars in county contracts in recent years.” In the 16th paragraph, on the second page of the story, Newsday cites Levy and his wife as saying she did not work on county business for the firms.
“This inaccurate and irresponsible series of articles [goes] to great lengths to insinuate that Colleen built her businesses upon my becoming county executive, and that she and I have somehow attempted to avoid proper disclosure,” Levy said in a July 2010 statement. In an interview, Levy called it “disgraceful reporting with numerous inaccuracies.”
In the case of a July 31 article, “Babylon lawyer to head group probing ethics commission,” Levy said it contains a “gross misrepresentation” of what is required to be listed on state financial disclosure forms. The state form requires the filer to list his or her sources of income and those of a spouse. However, the form says, “Do not list the name of individual clients, customers or patients.” The county form does not require the filer to list clients either.
In the July 31 article, the reporter writes, “Newsday reported earlier this month that court reporting firms owned by Levy’s wife, Colleen West, do business with at least seven county vendors that have received millions in payments from the county. Levy said he is not required to disclose his wife’s clients, even though the county form requires disclosing all sources of income, including those of a spouse.”
Levy takes issue with the story painting the picture that disclosing his wife’s clients and disclosing his wife’s income are one and the same. He also said, “Shockingly, Newsday failed to note that the county form likewise does not require or request a listing of individual clients,” and that this omission suggests that by filing the state form, he was attempting to hide information from the public.
In addition, in “A question of disclosure,” the Newsday reporter writes that in 2008 County Attorney Christine Malafi, at Levy’s request, wrote a letter to law firms receiving county business, making it clear that Enright was not on a list of court reporters that could be chosen for county business. Newsday said this was after the PBA raised questions about Enright doing county work. However, Levy said in an interview that it was in 2005, through Malafi, that he notified all county vendors that would use court reporting services that they were only to use the firm that was awarded the county bid, which was not Enright.
Concerned by the coverage, Levy said he presented Newsday several times with memos refuting information in various stories on several topics. Newsday did print a correction following an October 2010 story alleging Levy redacted personal financial information from his disclosure forms, when the Suffolk County Ethics Commission had actually redacted the information. But Levy said his concerns were largely limited to the letters page, instead of in further news reports or corrections.
In May 2011, the Press Club of Long Island announced Newsday’s main reporter on these stories won Outstanding Long Island Journalist. In 2009 the reporter, along with another Newsday reporter, won the Selden Ring Award for Investigative Reporting for a series of articles about special government districts.
The past, present and future
Levy said he made enemies because he “made tough decisions” — reorganizing the police department to save money, selling the Foley nursing home, limiting county hires and requiring union givebacks as a way to avoid county layoffs.
A fiscal conservative, Levy prided himself on saving money where he could. He said he gave up three bodyguards, took 240 county cars out of service, which had been “doled out like political lollipops.” He said his administration developed a different mind-set for county government, requiring double sign-offs for overtime and controlling travel expenditures. The county put its health care package out to competitive bid and saved $18 million annually, Levy said.
“Despite the tough times we’re having, we’re still in better shape than [surrounding counties] are and that’s because of the foundation that we’ve laid out over these many years. But it’s certainly not going to be easygoing into the next couple of years until the national economy picks up again.”
He doesn’t regret his run for governor, rather he said he would have been kicking himself if he hadn’t tried. He doesn’t regret his party change either, although he said it made him more of a target than when he was a Democrat. Levy said his switch to the Republican Party was not an act of political opportunism, having received endorsements of the Republican and Conservative parties; he won cross-party endorsements for his second term as county executive starting January 2008, winning 96 percent of the vote. The county executive had always leaned to the right economically and on the topic of immigration.
“It wasn’t a big leap, it wasn’t such a surprise to people in Suffolk,” Levy said.
But within one year of switching parties and announcing his run for governor, Levy made a deal with DA Spota to give back the $4 million in campaign funds and not seek re-election for a third term — ending his tenure under what many have called a cloud of suspicion.
Although he was forthcoming about other controversial issues, the county executive was tight-lipped about his agreement with Spota. He simply said, “We’ll have that conversation at another time.”