SBU scientists explore racial differences in GI cancers
It’s a dream team tackling a nightmare scenario. While colorectal and pancreatic cancers are killers across different races, they are considerably worse for African Americans.
African Americans with colorectal cancer are about 40 percent more likely to die from it compared to those from other racial groups, according to recent data from the Surveillance, Epidemiology and End Results Program. The incidence of pancreatic cancer in African Americans is also 31 to 65 percent higher than in other racial groups.
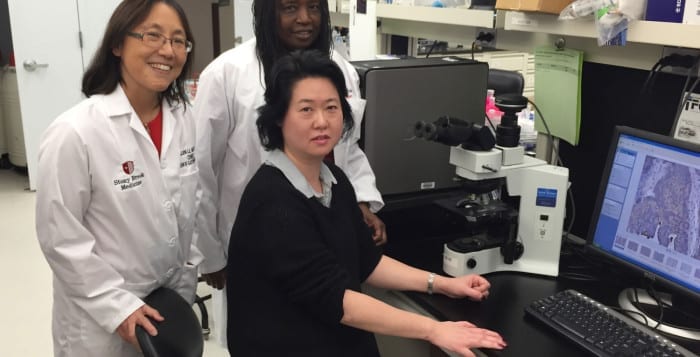
A Stony Brook University research team led by Ellen Li, a professor of medicine and chief of the Division of Gastroenterology and Hepatology, is trying to understand the causes of these variations and, in the process, hopes to provide the kinds of clinical benefits that would help everyone.
“We think there are multiple factors,” Li said. Scientists at Stony Brook, Cold Spring Harbor Laboratory and SUNY Downstate Health Disparities Center are creating one of “the most comprehensive data sets” that people can analyze.
The team includes Jennie Williams, an associate professor in the Department of Family, Population and Preventive Medicine, Joel Saltz, the chair of Bioinformatics at Stony Brook, Richard McCombie, director of the Stanley Institute for Cognitive Genomics at Cold Spring Harbor Laboratory, David Tuveson, the director of the Lustgarten Foundation Pancreatic Research Laboratory at CSHL and several other researchers at Downstate.
Williams said she began reading up on the response to cancer treatment by various groups in 2004. She understood that African Americans don’t respond to numerous chemotherapy prevention agents and some treatments for colon cancer. “They either don’t respond or they become resistant to chemotherapy,” she said.
When Williams started looking into this in 2008, she focused on microRNAs, which bind to messenger RNA and suppress translation. MicroRNAs are noncoding regulatory RNAs. The dysregulation of these important sequences result in the silencing of tumor suppressor proteins and the overexpression of oncogenes.
Her biggest finding was that the expression of tumor suppressor proteins inversely correlated with the overexpression of a microRNA called miR-182. This microRNA, she said, was significantly higher in tumor samples from African Americans.
With a molecular target and a potential mechanism, Williams thought she was well on her way to digging in. She ran into a significant stumbling block, however. “To do cancer chemotherapeutic studies, you need cell lines to work with,” she said.
Williams went to several companies to find colon cancer cell lines and asked, specifically, for those from African American patients. She found that the only cell lines labeled with race were those from Caucasians.
“To study chemoresponse, one needs a broad spectrum of cell lines,” Williams said.
She started generating cell lines in her lab, with three from African Americans and two from Hispanic patients, as well as some from Caucasians.
While Williams said she loves living in Stony Brook, she has found the lack of diversity among the patient population limiting in addressing cancer racial disparity. With Li’s help, she partnered with Downstate, where 75 percent of the patient population is African American.
She hopes to generate 10 African American, 10 Hispanic American and 10 Caucasian cell lines. Stony Brook and Downstate will collaborate to exchange ideas and personnel.
Williams said part of the challenge in gathering tissue samples from the African American population comes from a history of worrisome interactions with scientists.
Many African Americans have heard of the Tuskegee Institute study of African American men who came to the institute with syphilis between 1932 and 1972 but were not treated with penicillin, even after the drug became an effective and standard treatment in 1947. When the public became aware of the study, it ended and the government established strict informed consent rules about participating in scientific research.
Li said in their study on racial disparities in gastrointestinal cancers, selected staff certified in human research de-identifies everything so no one knows who each participant is. The data collection is a labor-intensive work, Li said, that is designed to provide greater insight into what might be causing these differences.
In terms of explaining the differences, Li and Williams believe it is both “genetic and epigenetic.”
In Africa, colon cancer is rare compared to its occurrence in the United States, Williams said, which suggests that diet and lifestyle contribute to the disease and its progression.
Raised in Savannah, Georgia, Williams said she was always interested in what made things change, from the tadpole in the pond to insects and birds that flew. While her parents didn’t attend college, that wasn’t an option for her: “It was never if” she went to college, “but when.”
Li, who is married to Stony Brook President Sam Stanley and has four children, said health insurance is one of numerous problems that affect individual populations. Numerous other factors could play a role in explaining the racial disparities in cancer outcomes.
Diabetes, which occurs at a higher rate in African Americans, increases the risk of colon cancer, Li said. It is unclear how much the incidence of diabetes in the African American population may contribute to the disparity, Li said.