By David Dunaief, M.D.

Our assumptions about alcohol and health are complicated and often wrong. Many of you may have heard that Europeans who drink wine regularly live longer because of this. Or that only heavy drinkers need to be concerned about long-term health impacts. Would it surprise you to hear that both assumptions have been studied extensively?
Alcohol is one of the most widely used over-the-counter drugs, and yet there is still confusion over whether it benefits or harms to your health. The short answer: it depends on your circumstances, including your family history and consideration of diseases you are at high risk of developing, including cancers, heart disease and stroke.
Alcohol and cancer risk
The National Cancer Institute notes that alcohol is listed as a known carcinogen by the National Toxicology Program of the US Department of Health and Human Services (1). Among the research it details, it lists head and neck, esophageal, breast, liver and colorectal cancers as key cancer risks that are increased by alcohol consumption. Of these, esophageal and breast cancer risks are increased with even light drinking. Let’s look more closely at some of the research on breast cancer risk that supports this.
A meta-analysis of 113 studies found there was an increased risk of breast cancer with daily alcohol consumption (2). The increase was a modest, but statistically significant, four percent, and the effect was seen at one drink or fewer a day. The authors warned that women who are at high risk of breast cancer should not drink alcohol or should drink it only occasionally.
It was also shown in the Nurses’ Health Study that drinking three to six glasses a week increased the risk of breast cancer modestly over a 28-year period (3). This study involved over 100,000 women. Even a half-glass of alcohol was associated with a 15 percent elevated risk of invasive breast cancer. The risk was dose-dependent, meaning the more participants drank in a day, the greater their risk increase. In this study, there was no difference in risk by type of alcohol consumed, whether wine, beer or liquor.
Based on what we think we know, if you are going to drink, a drink a few times a week may have the least impact on breast cancer. According to an accompanying editorial, alcohol may work by increasing the levels of sex hormones, including estrogen, and we don’t know if stopping diminishes this effect (4).
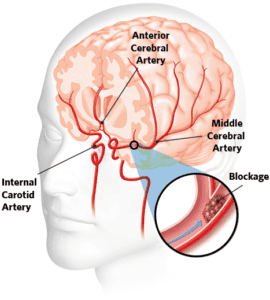
Alcohol and stroke risk
On the positive side, the Nurses’ Health Study demonstrated a decrease in the risk of both ischemic (caused by clots) and hemorrhagic (caused by bleeding) strokes with low to moderate amounts of alcohol (5). This analysis involved over 83,000 women. Those who drank less than a half-glass of alcohol daily were 17 percent less likely than nondrinkers to experience a stroke. Those who consumed one-half to one-and-a-half glasses a day had a 23 percent decreased risk of stroke, compared to nondrinkers.
However, women who consumed more experienced a decline in benefits, and drinking three or more glasses daily resulted in a non-significant increased risk of stroke. The reasons for alcohol’s benefits in stroke have been postulated to involve an anti-platelet effect (preventing clots) and increasing HDL (“good”) cholesterol. Patients should not drink alcohol solely to get stroke protection benefits.
If you’re looking for another option to achieve the same benefits, an analysis of the Nurses’ Health Study recently showed that those who consumed more citrus fruits had approximately a 19 percent reduction in stroke risk (6). The citrus fruits used most often in this study were oranges and grapefruits. Note that grapefruit may interfere with medications such as Plavix (clopidogrel), a commonly used antiplatelet medication used to prevent strokes (7).
Alcohol and heart attack risk
In the Health Professionals follow-up study, there was a substantial decrease in the risk of death after a heart attack from any cause, including heart disease, in men who drank moderate amounts of alcohol compared to those who drank more and those who were non-drinkers (8). Those who drank less than one glass daily experienced a 22 percent risk reduction, while those who drank one-to-two glasses saw a 34 percent risk reduction. The authors mention that binge drinking negates any benefits.
What’s the conclusion?
Moderation is the key. It is important to remember that alcohol is a drug, and it does have side effects, including insomnia. The American Heart Association recommends that women drink up to one glass a day of alcohol. I would say that less is more. To achieve the stroke benefits and avoid increased breast cancer risk, half a glass of alcohol per day may work for women. For men, up to two glasses daily counts as moderate, though one glass showed significant general health benefits.
If you choose to forgo alcohol, the good news is that there is a growing variety of non-alcoholic beverages entering the market and increasing in popularity.
References:
(1) cancer.gov. (2) Alc and Alcoholism. 2012;47(3)3:204–212. (3) JAMA. 2011;306:1884-1890. (4) JAMA. 2011;306(17):1920-1921. (5) Stroke. 2012;43:939–945. (6) Stroke. 2012;43:946–951. (7) Medscape.com. (8) Eur Heart J. Published online March 28, 2012.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.