By Daniel Dunaief
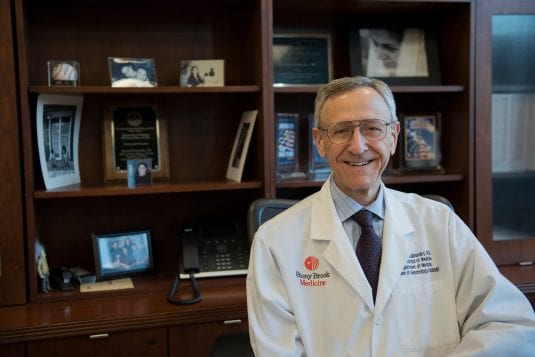
Like so many others, Ken Kaushansky had to alter his plans when the pandemic hit last March. Kaushansky had expected to retire after over 10 years as Dean of the Renaissance School of Medicine at Stony Brook University and the Senior Vice President of Health Sciences, but the public health needs of the moment, particularly on Long Island which became an early epicenter for the disease, demanded his attention.
“Now that COVID hopefully is coming under control, it seems more logical” to retire this year, Kaushansky said in a wide-ranging interview about the pandemic, his career, and the medical school. In January, he stepped down as the dean, while he plans to retire as Senior Vice President of Health Sciences at the end of June.
Views on the Pandemic
Looking back at the immediate challenges in the first few months, Kaushansky said SBU did “extremely well” in caring for patients who were battling COVID-19 and was gratified by the school’s effort to catalog and understand the disease. “I’m very proud that we’ve been able to study this infection on all sorts of levels and make a real impact that has helped others,” he said.
Early on, as the medical team at Stony Brook met, Kaushansky urged the hospital to study COVID “to the hilt” and to “extract every little bit of data we can. We must keep all that data on all these patients.”
Indeed, Stony Brook has created a database that continues to grow of close to 10,000 people, which includes 3,000 inpatients, 4,000 who weren’t sick enough for hospital admission, and around 3,000 who thought they had the disease, but had other illnesses. “We’ve learned a ton from that, and it’s not just learning for learning’s sake,” Kaushansky said. The demand for the use of the database is so high that a steering committee is reviewing proposals.
Stony Brook had heard from doctors in Italy that COVID patients were having problems with blood clotting. This symptom was particularly meaningful to Kaushansky, who is a hematologist.
SBU studied the symptoms and “did a trial to see if aggressive anticoagulants would produce better outcomes” than the standard of care at the time, he said. “Our [intensive care unit] patients who were on this more aggressive anticoagulation protocols had half the mortality” of other patients, so the hospital “quickly adopted all of our care” to the more effective approach.
The hospital preemptively used biomarkers to determine who should and should not get aggressive anticoagulation. A subsequent study using the database confirmed the school’s early conclusion. Stony Brook published over 150 papers on the structure of the virus, clinical observations, sociological interventions, and a host of other areas, according to Kaushansky.
Carol Gomes, Chief Executive Officer of Stony Brook University Hospital, appreciated Kaushansky’s hands on approach, which included participating in daily calls as part of the hospital incident command center.
She likened Kaushansky to an orchestra leader, coordinating the research and patient care, making sure there was “no duplication of effort.”
Kaushansky believes federal research funding agencies and policy makers will recognize the importance of gathering information about this pandemic to treat future patients who might battle against variants and to provide a playbook for other health threats. “We really do need to prepare for the next one” as this is the third and deadliest of three coronaviruses, including SARS and MERS, he said.
Vaccines
As for vaccines, Kaushansky said Stony Brook was making it as “convenient as we can” to get a vaccination for health care workers. As of about a month ago, over 80 percent of Stony Brook’s health care workers had been vaccinated.
The black and brown communities have benefited from seeing leaders and role models receiving the vaccine. “This is beginning to erode the mistrust,” said Kaushansky, which developed as a byproduct of the infamous Tuskegee experiment, in which black men with syphilis did not receive penicillin despite its availability as an effective treatment.
Kaushansky added that a concern he’s heard from a range of people is that the vaccine was developed too quickly and that the side effects could be problematic. He cited the simultaneous steps doctors, pharmaceutical companies and others took to accelerate a process that didn’t leave out any of those steps.
Kaushansky participates in a group email interaction with prominent European hematologists. Looking at the data for the Astrazeneca vaccine, these researchers have calculated that anywhere from one in 500,000 to one in a million have developed blood clots.
“Not a single person on this mass email believes that they should stop the Astrazeneca vaccines for that kind of incident,” he said.
What He Helped Build
Kaushansky has been such a supporter of expanding the facilities and expertise at Stony Brook that he said the campus developed a joke about him.
“What’s the dean’s favorite bird?” he asked. “A crane.”
Fixtures on the campus for years, those cranes — the construction vehicles, not the birds — have changed the university, adding new teaching, research and clinical space on the campus.
That includes the Medical and Research Translational building and Bed Tower, which started in 2013 and opened in 2018, and the Hospital Pavilion, which has an additional 150 beds. Those extra beds were especially important a year after the pavilion opened, providing much-needed space for patients battling against COVID.
Gomes appreciated what Kaushansky built physically, as well as the interactive collaborations among different parts of the university. “An active collaboration and communication between researchers, clinicians and academics is a very different model” from the typical separation among those groups, she said. The work “reaped great rewards on the front end with the ability to collaborate to bring new ideas forward.”
As for the type of care patients received at Stony Brook, Kaushansky recalled a discussion over six years ago about central line infections. The data came from a 12 month period, starting six months prior to the meeting and going back to 18 months earlier.
“How are we going to know why all those central line infections occurred by looking at data” from so much earlier, Kaushansky recalled asking. The hospital created real time dashboards, which is an effort that has “paid huge dividends.”
Kaushansky cited the hospitals’ top 100 health grade for three years running. These grades assess whether patients survive a procedure, have complications or need to be readmitted.
“You’re going to get the best care possible when you come to Stony Brook,” Kaushansky said, as the top 100 rating puts Stony Brook in the top 2 percent of hospitals in the country.
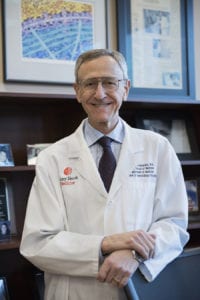
Apart from the buildings Kaushansky helped develop, he’s proud of the program he helped build for medical school students.
About six years ago, Stony Brook instituted a new medical school curriculum that had translational pillars. The school starts students in the clinical realm considerably earlier than the classic program that involves two years of basic studies, followed by two years of clinical work.
Stony Brook provides basic science, followed by earlier exposure to the clinic, with a return to basic science after that
“It’s much more effective if you teach the basic science after the student has witnessed the clinical manifestation,” Kaushansky said. These approaches are part of translational pillars in areas such as cancer, physiology and infectious diseases.
As for what he’ll miss after he leaves, Kaushansky particularly appreciated the opportunity to speak with students. He used to hold a monthly breakfast with four or five students, where he learned about each student, their career goals and their medical journey.
A former colleague at the University of California at San Diego, John Carethers, who is the Chair in the Department of Internal Medicine at the University of Michigan, visited Kaushansky as a speaker twice at Stony Brook.
Carethers saw “first hand the wonderful impact he had on students — knowing their names, and providing wonderful advice,” he wrote in an email.
The Next Steps
For a decade, Kaushansky said he wanted to create a course about the future of medicine.
“There are a lot of great innovations in medicine that are fascinating from a scientific and clinical perspective,” Kaushansky said.
He will work on a course for use at Stony Brook in the main campus, the medical campus and for whichever program is interested in sharing these innovative medical and scientific steps in medicine.
He also plans to continue to be the lead editor of the primary textbook in hematology, called Williams Hematology. The textbook has gone through 10 editions.
Kaushansky and his wife Lauren, who is an author and education professor at Stony Brook, aren’t likely to remain on Long Island in the longer term. The couple has a getaway home in Santa Fe and may go there.
Kaushansky’s hobbies include wood working and running. He made a sofa when he was an undergraduate at UCLA, while his second significant work was a 16-foot sailboat he made as a second-year resident. He estimates he has made 40 pieces of furniture.
Kaushansky runs four miles a day four to six times a week. In 1990, he ran the Seattle Marathon which was the Goodwill Games Marathon, finishing in a time of around three hours and twenty-five minutes.
Culturally, Kaushansky hopes the school continues to embrace his focus on generosity.
“You’ve got to be generous with your time,” he said.
“No more can you say that you are too busy to talk. You have to be of a personality that takes pride and that gets the endorphins going from seeing the people you have brought, the people you have entrusted in leadership roles, succeed.”
Photos courtesy of Stony Brook University