By David Dunaief, M.D.

Heart disease gets a lot of attention, because it’s still the number one cause of death in the U.S. We know that diet plays a significant role in this, but so do our genes.
What if we could tackle genetic issues with diet?
A study involving the Paleo-type diet and other ancient diets suggests that there is a significant genetic component to cardiovascular disease, while another study looking at the Mediterranean-type diet implies that we may be able to reduce our risk factors with lifestyle adjustments. Most of the risk factors for heart disease, such as high blood pressure, high cholesterol, sedentary lifestyle, diabetes, smoking and obesity are modifiable (1). Let’s look at the evidence.
The role of genes
Researchers used computed tomography scans to look at 137 mummies from ancient times across the world, including Egypt, Peru, the Aleutian Islands and Southwestern America (2). The cultures were diverse, including hunter-gatherers (consumers of a Paleo-type diet), farmer-gatherers and solely farmers. Their diets were not vegetarian; they involved significant amounts of animal protein, such as fish and cattle.
Researchers found that one-third of these mummies had atherosclerosis (plaques in the arteries), which is a precursor to heart disease. The ratio should sound familiar. It aligns with what we see in modern times.
The authors concluded that atherosclerosis could be part of the aging process in humans. In other words, it may be a result of our genes. Being human, we all have a genetic propensity toward atherosclerosis and heart disease, some more than others, but many of us can reduce our risk factors significantly.
I am not saying that the Paleo-type diet specifically is not beneficial compared to the standard American diet. Rather, that this study does not support that. However, other studies demonstrate that we can reduce our chances of getting heart disease with lifestyle changes, such as with a plant-rich diet, such as a Mediterranean-type diet.
Can we improve our genetic response with diet?
The New England Journal of Medicine published study about the Mediterranean-type diet and its potential impact on cardiovascular disease risk (3). Here, two variations on the Mediterranean-type diet were compared to a low-fat diet. People were randomly assigned to three different groups. The two Mediterranean-type diet groups both showed about a 30 percent reduction in the risk of cardiovascular disease, compared to the low-fat diet. Study end points included heart attacks, strokes and mortality. Interestingly, the risk profile improvement occurred even though there was no significant weight loss.
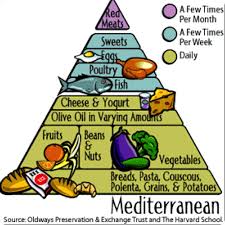
The Mediterranean-type diets both consisted of significant amounts of fruits, vegetables, nuts, beans, fish, olive oil and wine. I call them “Mediterranean diets with opulence,” because both groups consuming this diet had either significant amounts of nuts or olive oil and/or wine. If the participants in the Mediterranean diet groups drank wine, they were encouraged to drink at least one glass a day.
The study included three groups: a Mediterranean diet supplemented with mixed nuts (almonds, hazelnuts or walnuts), a Mediterranean diet supplemented with extra virgin olive oil (at least four tablespoons a day), and a low-fat control diet. The patient population included over 7,000 participants in Spain at high risk for cardiovascular disease.
The strength of this study, beyond its high-risk population and its large size, was that it was a randomized clinical trial, the gold standard of trials. However, there was a significant flaw, and the results need to be tempered. The group assigned to the low-fat diet was not, in fact, able to maintain this diet throughout the study. Therefore, it really became a comparison between variations on the Mediterranean diet and a standard diet.
What do the leaders in the field of cardiovascular disease and integrative medicine think of the Mediterranean diet study? Interestingly there are two opposing opinions, split by field. You may be surprised by which group liked it and which did not.
Cardiologists, including well-known physicians Henry Black, M.D., who specializes in high blood pressure, and Eric Topol, M.D., former chairman of cardiovascular medicine at Cleveland Clinic, hailed the study as a great achievement. This group of physicians emphasized that now there is a large, randomized trial measuring clinical outcomes, such as heart attacks, stroke and death.
On the other hand, the integrative medicine physicians, Caldwell Esselstyn, M.D., and Dean Ornish, M.D., both of whom stress a plant-rich diet that may be significantly more nutrient dense than the Mediterranean diet in the study, expressed disappointment with the results. They feel that heart disease and its risk factors can be reversed, not just reduced. Both clinicians have published small, well-designed studies showing significant benefits from plant-based diets (4, 5). Ornish actually showed a reversal of atherosclerosis in one of his studies (6).
So, who is correct about the Mediterranean diet? Each opinion has its merits. The cardiologists’ enthusiasm is warranted, because a Mediterranean diet, even one of “opulence,” will appeal to more participants, who will then realize the benefits. However, those who follow a more focused diet, with greater amounts of nutrient-dense foods, will potentially see a reversal in heart disease, minimizing risk — and not just reducing it.
So, what have we learned? Even with a genetic proclivity toward cardiovascular disease, we can alter our cardiovascular destinies.
References:
(1) www.uptodate.com. (2) BMJ 2013;346:f1591. (3) N Engl J Med 2018; 378:e34. (4) J Fam Pract. 1995;41(6):560-568. (5) Am J Cardiol. 2011;108:498-507. (6) JAMA. 1998 Dec 16;280(23):2001-2007.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com.