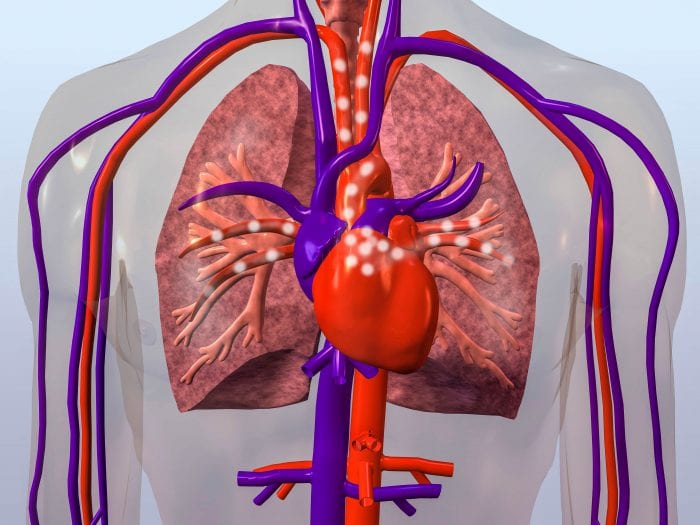
Lung health is affected by simple diet and exercise changes
By David Dunaief, M.D.

The COVID-19 pandemic has raised many people’s awareness of the importance of lung function. Its consequences are especially severe for those with chronic obstructive lung diseases such as chronic obstructive pulmonary disease (COPD) and asthma, as well as those who smoke and vape.
What can we do to strengthen our lungs? We can improve lung function with simple lifestyle modifications including exercising, eating a plant-based diet with a focus on fruits and vegetables, expanding lung capacity with an incentive spirometer, and quitting smoking and vaping, which damage the lungs (1). Not only people with compromised lungs will benefit; studies suggest everyone will benefit.
COPD and diet
Several studies demonstrate that higher consumption of fiber from plants decreases the risk of COPD in smokers and ex-smokers. Bear with me, because the studies were done with men or women, not both at the same time. In one study of men, for example, results showed that higher fiber intake was associated with significant 48 percent reductions in COPD incidence in smokers and 38 percent incidence reductions in ex-smokers (3). The high-fiber group ate at least 36.8 grams per day, compared to the low-fiber group, which ate less than 23.7 grams per day. Fiber sources were fruits, vegetables and whole grain, essentially a whole foods plant-based diet. The high-fiber group was still below the American Dietetic Association-recommended 38 grams per day. This is within our grasp.
In another study, women had a highly significant 37 percent decreased risk of COPD among those who consumed at least 2.5 serving of fruit per day compared to those who consumed less than 0.8 servings per day (4). The highlighted fruits shown to reduce COPD in both men and women included apples, bananas, and pears.
Asthma and diet
In a randomized controlled trial of asthma patients, results show that after 14 days those who ate a low-antioxidant diet had less lung function compared to those who ate a high-antioxidant diet (2). Researchers measured lung function with one-second forced expiratory volume (FEV1) and predicted forced vital capacity (FVC).
Additionally, those who were in the low-antioxidant diet group also had higher inflammation at 14 weeks, as measured using a c-reactive protein (CRP) biomarker. Those who were in the low-antioxidant group also were over two-times more likely to have an asthma exacerbation.
The good news is that the difference in behavior between the high- and low-antioxidant groups was small. The high-antioxidant group had a modest five servings of vegetables and two servings of fruit daily, while the low-antioxidant group ate no more than two servings of vegetables and one serving of fruit daily.
Carotenoid supplementation, instead of antioxidant foods, made no difference in inflammation. The authors concluded that an increase in carotenoids from diet has a clinically significant impact on asthma and can be seen in a very short period.
Incentive spirometry
What is an incentive spirometer? It’s a device that helps expand the lungs by inhaling through a tube and causing a ball or multiple balls to rise. This opens the alveoli and may help you breathe better.
Incentive spirometry has been used for patients with pneumonia, those who have chest or abdominal surgery and those with asthma or COPD, but it has also been useful for healthy participants (5). A small study showed that those who trained with an incentive spirometer for two weeks increased their vital capacity, right and left chest wall motion, and right diaphragm motion. This means it improved lung function and respiratory motion. Participants were 10 non-smoking healthy adults who were instructed to take five sets of five deep breaths twice a day, totaling 50 deep breaths per day. The brands used in the study are inexpensive and easily accessible, such as Teleflex’s Triflo II.
In another small, two-month study of 27 patients with COPD, the incentive spirometer improved blood gasses, such as partial pressure carbon dioxide and oxygen, in COPD patients with exacerbation (6). The authors concluded that it may improve quality of life for COPD patients.
Exercise
Exercise can have a direct impact on lung function. In a study involving healthy women ages 65 years and older, results showed that 20 minutes of high-intensity exercise three times a day improved FEV1 and FVC, both indicators of lung function, in as little as 12 weeks (7). Participants began with a 15-minute warm-up, then 20 minutes of high-intensity exercise on a treadmill, followed by 15 minutes of cool-down with stretching.
What is impressive is that it was done in older adults, not those in their twenties and not in elite athletes.
Note that you don’t need a treadmill to do aerobic exercise. You can walk up steps or steep hills in your neighborhood, do jumping jacks, or even dance in your living room. Whatever you choose, you want to increase your heart rate and expand your lungs. If this is new for you, consult a physician and start slowly. You’ll find that your stamina improves rather quickly over time.
We all should be working to strengthen our lungs, regardless of COVID-19. This three-pronged approach of lifestyle modifications – diet, exercise and incentive spirometer – can help without expending significant time or expense.
References:
(1) Public Health Rep. 2011 Mar-Apr; 126(2): 158-159. (2) Am J Clin Nutr. 2012 Sep;96(3):534-43.(3)Epidemiology Mar 2018;29(2):254-260. (4)Int J Epidemiol Dec 1 2018;47(6);1897-1909. (5)Ann Rehabil Med. Jun 2015;39(3):360-365. (6)Respirology. Jun 2005;10(3):349-53.(7)J Phys Ther Sci. Aug 2017;29(8):1454-1457.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com.