Cortisol resistance can increase susceptibility to viruses and infection
By David Dunaief, M.D.

This has been a tough year, where many of us have been under continual stress. While some stress is valuable to help motivate us and keep our minds sharp, high levels of constant stress can have detrimental effects on the body.
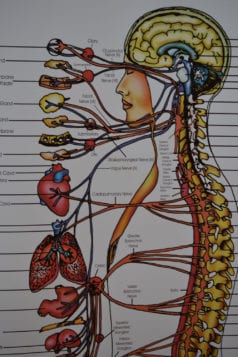
Nowhere is the mind-body connection clearer: although stress may start in the mind, it can lead to acute or chronic disease promotion. It can also play a role with your emotions, causing irritability and outbursts of anger and possibly leading to depression and anxiety.
Stress symptoms can include stiff neck, headaches, stomach upset and difficulty sleeping. Stress may also be associated with cardiovascular disease, with an increased susceptibility to infection from viruses causing the common cold, and with cognitive decline and Alzheimer’s (1).
A stress steroid hormone, cortisol, is released from the adrenal glands and can have beneficial effects in small bursts. We need cortisol in order to survive. Some of its functions include raising glucose (sugar) levels when they are low and helping reduce inflammation and stress levels (2). However, when cortisol gets out of hand, higher chronic levels may cause inflammation, leading to disorders such as cardiovascular disease, as research suggests.
Let’s look at the evidence.
Inflammation
Inflammation may be a significant contributor to more than 80 percent of chronic diseases. In a meta-analysis (a group of two observational studies), high levels of C-reactive protein (CRP), a biomarker for inflammation, were associated with increased psychological stress (3).
A study of over 73,000 adults found that with CRP higher than 3.0 there was a greater than twofold increase in depression risk. The researchers suggest that CRP may heighten stress and depression risk by increasing levels of inflammatory communicators among cells (4).
In one study, results suggested that stress may influence and increase the number of hematopoietic stem cells (those that develop all forms of blood cells), resulting specifically in an increase in inflammatory white blood cells (5). The researchers suggest that this may lead to these white blood cells accumulating in atherosclerotic plaques in the arteries, which ultimately could potentially increase the risk of heart attacks and strokes. Chronic stress overactivates the sympathetic nervous system — our “fight or flight” response — which may alter the bone marrow where the stem cells are found. This research is preliminary and needs well-controlled trials to confirm these results.
Infection
Stress may increase the risk of colds and infection. Over the short term, cortisol is important to help suppress the symptoms of colds, such as sneezing, cough and fever. These are visible signs of the immune system’s infection-fighting response. However, the body may become resistant to the effects of cortisol, similar to how a type 2 diabetes patient becomes resistant to insulin.
In one study of 296 healthy individuals, participants who had stressful events and were then exposed to viruses had a higher probability of catching a cold. It turns out that these individuals also had resistance to the effects of cortisol. This is important because those who were resistant to cortisol had more cold symptoms and more proinflammatory cytokines (6).
Lifestyle changes can reduce effects of stress
Lifestyle plays an important role in stress at the cellular level, specifically at the level of the telomere, which determines cell survival. The telomeres are to cells as the plastic tips are to shoelaces; they prevent them from falling apart. The longer the telomere, the slower the cell ages and the longer it survives.
In a one-year study of women aged 50 to 65, those who followed a healthy lifestyle — one standard deviation over the average lifestyle — were able to withstand life stressors better since they had longer telomeres (7). This healthy lifestyle included regular exercise, a healthy diet and a sufficient amount of sleep. On the other hand, the researchers indicated that those who had poor lifestyle habits lost substantially more telomere length than the healthy lifestyle group.
In another study, chronic stress and poor diet (high sugar and high fat) together increased metabolic risks, such as insulin resistance, oxidative stress and central obesity, more than a low-stress group eating a similar diet (8). The high-stress group members were caregivers, specifically those caring for a spouse or parent with dementia. This is a good reminder that it’s especially important to eat a healthy diet when under stress.
Interestingly, in terms of sleep, the Evolution of Pathways to Insomnia Cohort (EPIC) study shows that those who deal directly with stressful events are more likely to have good sleep quality. Using medication, alcohol or, most surprisingly, distractors, such as television watching or other activities, to deal with stress all resulted in insomnia after being followed for one year (9). Cognitive intrusions or repeat thoughts about the stressor also resulted in insomnia.
The most important message from this study is that how a person reacts to and deals with stressors may determine whether they suffer from insomnia.
We need to recognize the effects of constant stress. If it’s not addressed, it can lead to suppressed immune response or increased levels of inflammation. To address chronic stress and lower CRP, it is important to adopt a healthy lifestyle that includes sleep, exercise and diet modifications. Good lifestyle habits may also be protective against the effects of stress on cell aging.
References:
(1) Curr Top Behav Neurosci. 2014 Aug. 29. (2) Am J Physiol. 1991;260(6 Part 1):E927-E932. (3) JAMA Psychiatry. 2013;70:176-184. (4) Chest. 2000;118:503-508. (5) Nat Med. 2014;20:754-758. (6) Proc Natl Acad Sci U S A. 2012;109:5995-5999. (7) Mol Psychiatry Online. 2014 July 29. (8) Psychoneuroendocrinol Online. 2014 April 12. (9) Sleep. 2014;37:1199-1208.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com.