SBU’s Lebowitz suggests test scores only one piece in diagnosis puzzle
What, exactly, do test results mean? It is a question professionals in teaching, human resource and medicine grapple with routinely. A lower SAT score, for example, could reflect anything from a poor night’s sleep the night before, to a cold test room, to a lack of familiarity with the type and style of questions asked.
Similarly, doctors and researchers routinely use tests. Sometimes, the tests can show something specific, like a bone fracture or a break. Other times, however, the tests can leave room for interpretation, particularly if those tests involve processes that go on in a complex area, such as the mind.
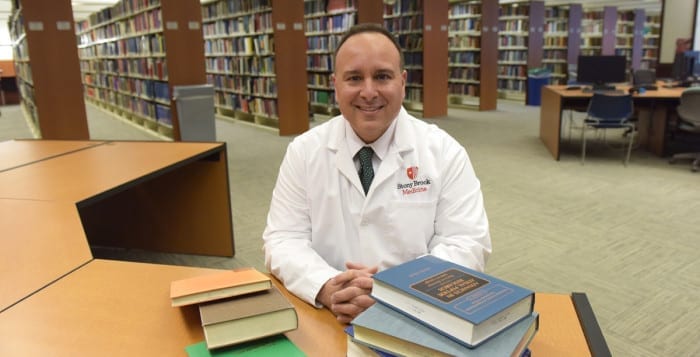
Brian K. Lebowitz, director of neuropsychology training and clinical assistant professor of neurology at Stony Brook University, recently showed that a cognitive test might incorrectly suggest signs of the type of problems associated with Alzheimer’s disease.
“It’s possible that people are mislabeled because if [they] have a lifelong cognitive weakness, they [might] perform poorly” on the test, Lebowitz said.
Generally, people who have memory problems, or so-called mild cognitive impairment, visit Lebowitz or other neuropsychologists to understand if they are developing age-related problems or a chronic challenge, like Alzheimer’s disease.
Previous conditions or difficulty learning, however, may complicate a diagnosis in interpreting scores on any cognitive evaluations.
“If you had difficulty with cognitive processes that led to reading disorders in childhood, in forming complex language at age eight,” you might have it at age 80, Lebowitz suggested. “Our study, as well as clinical experiences, suggests that this is the case.” This, he continued, “is exactly what we would like to know.”
Lebowitz recently published his analysis in the Journal of Alzheimer’s Disease.
“Some of the results on all different kinds of tests” can arise from different challenges because “different cognitive skill sets overlap,” said Thomas Preston, the director of Neuropsychology Service at Stony Brook. Lebowitz’s article on mild cognitive impairment can help those who work with patients gain a better understanding of a patient’s history “prior to any perceived decline.”
Lebowitz looked more closely at the possible connection between test scores and reading challenges after speaking extensively with adults who had performed poorly on reading tests.
“Often during the interview, a patient will indicate that they have always struggled with reading or that they were diagnosed with dyslexia,” Lebowitz said. “Based on the reported histories, it was clear that at least for some patients, cognitive test scores reflected longstanding difficulties.”
In more recent times, child psychologists and education professionals have focused on dyslexia and other reading difficulties. Around 50 years ago, assessing learning disorders was not part of the American educational system, said Lebowitz. “People may have been called slow learners or readers. If you were to ask an older adult if he had dyslexia, he’d have no idea,” he added.
Stony Brook’s neuropsychological assessment team sees a wide range of patients with difficulties that include dementia, stroke, people with vehicular brain injuries, cancer, tumors and numerous other challenges. They also see people with epilepsy and learning disabilities. Their patients range in age from pediatric to geriatric.
Lebowitz often provides information about why some people feel as though they are unable to succeed professionally or socially. With an older adult, he takes into account their life story, as well as their likely lifelong pattern of cognitive strengths and weaknesses, when interpreting test results, he said.
In addition to his research results and a good rapport with his patients, Lebowitz has helped reduce the evaluation time needed for adults, Preston said.
“He has a thorough but efficient method of evaluating” patients, Preston said. “Dr. Lebowitz has brought a new type of efficiency.” At one point, the typical neuropsychological evaluation could take as long as eight hours. That can now take two and a half hours, Preston said.
Lebowitz has been at Stony Brook for eight years and lives in Poquott with his 13-year-old Labrador retriever Japhy, whom he adopted as a rescue dog during his fellowship. For recreation, he enjoys taking a scuba diving trip each year. After returning from a trip to the Galapagos Islands in December he said, “every dive in the Galapagos was the best dive I’ve ever done.”
As for his recent research article, Lebowitz recognizes that there’s still considerable work to do to understand how to connect tests with diagnoses and treatment, particularly for mild cognitive impairment that might suggest Alzheimer’s.
“The challenge for all health care professionals who work with older adults is to identify cognitive decline at the earliest possible point,” he said. “As treatment options become available, identifying and treating patients before symptoms progress will be even more important.”
At this point, Lebowitz said he doesn’t know if he’s identified people who are being mislabeled as mild cognitive impairment because he has yet to follow them over time. People with a lifelong weakness “may be vulnerable to brain changes later in life.”
Still, these results highlight why it’s important for medical professionals to take into account a complete history in developing a diagnosis, instead of relying on a score on a particular test, he said.