CSHL’s Vakoc taps into bacterial system to battle cancer
We create buildings that climb into a sky crowded with airplanes and supersonic jets. We harness the energy of the atom, design intricate artwork, compose and perform inspirational music, travel miles below the surface of the ocean and send satellites deep into space. Sometimes, we tap into unlikely sources to learn new ways to improve our lives, even in the fight to understand and attack cancer.
Bacteria have been battling against viruses for so long that they have evolved to disarm these intruders. The bacterial immune system uses a gene-editing system called CRISPR. Researchers have taken some of the CRISPR machinery from bacteria and are using it in human cells. CRISPR was named the American Association for the Advancement of Science’s Breakthrough of the Year for 2015.
Using a bacterial enzyme called Cas9, which isn’t found naturally in humans but can be used in our genetic code, scientists can edit out DNA that contributes to the proliferation of cancer.
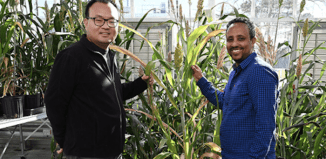
Christopher Vakoc, an associate professor at Cold Spring Harbor Laboratory, has used his expertise with CRISPR to study cancer.
Starting in the fall of 2014, he and Charles Keller, the scientific director at Children’s Cancer Therapy Development Institute in Oregon, collaborated to study the disease rhabdomyosarcoma, a rare form of deadly pediatric cancer of the connective tissue that typically involves muscle cells attached to bones. Vakoc’s lab is using CRISPR to discover new vulnerabilities in RMS.
At this point, Keller has found a potential treatment in animal models that shows positive results, while Vakoc has determined how that specific drug is working. They have submitted their work for publication in a scientific journal and are awaiting word back from reviewers.
Starting this fall, Vakoc will add Ph.D. scientist Bryan Lanning, who will try and identify new targets in RMS using CRISPR.
“It’s great to contribute more resources to this effort,” Vakoc said.
In an email, Keller detailed how “we have more insight into how the drug for rhabdomyosarcoma works.” He credits Eric Wang from Vakoc’s lab for contributing “instrumental” results to the early findings. Keller is “grateful for the support of [Vakoc’s] lab and the collaboration it empowers.”
At the same time, Vakoc’s lab continues to work in an area where they have made some breakthroughs with CRISPR, on a site called BRD4. Collaborating with several other labs, Vakoc showed that chemical inhibition of BRD4 provides a therapeutic benefit in mouse models of leukemia, which has led to clinical trials in humans. Using a drug called JQ1, scientists have generated positive results with humans in Phase I of the Food and Drug Administration’s process for therapeutic approval.

“Some of the patients at tolerated doses have had complete remission,” he said. He called those early findings “encouraging.”
A major area of focus, Vakoc explained, involves continuing to try to understand on a molecular level how these drugs are working and why BRD4 is a drug target. “It was not clear in the beginning, but we are slowly revealing the special properties of BRD4,” he said.
As the tests move into the next stage, called Phase 2, an important question in order for this therapy to work, Vakoc said, is to anticipate “how we are going to overcome these resistant states.”
While he doesn’t have an answer yet, he said, he hopes a combination of agents can be more active than any one treatment individually. “A lot of what we’ve been doing, while we are waiting for clinical trials to get under way, is to study resistance and therapies in animal and culture models,” Vakoc said.
Vakoc and Johannes Zuber, a group leader at the Research Institute of Molecular Pathology in Vienna, Austria, recently published a paper in which they outlined how some cells become resistant through nongenetic changes. As they described, the cells are rewiring gene expression without introducing new DNA. A cell can evolve to this new state, Vakoc said. In the battle to defeat the disease, this requires a readiness to defeat what he expects will be some level of resistance to this new treatment.
The inhibitors Vakoc and Zuber have worked on have “very broad and desired activity,” but to find a cure “we have to find effective combination therapies,” explained Zuber, who collaborated on BRD4 projects at Cold Spring Harbor when he was a postdoctoral researcher in Scott Lowe’s lab as early as 2008.
“Assuming that cancer drugs can be well-tolerated enough to be combined and administered as chronic therapy, I hold out hope that we can combine numerous agents and apply them upfront, based on information in the lab and real-life information from patients,” Vakoc said. This could mean a cocktail of three, four or five well-tolerated drugs that he hopes won’t increase chemotherapy toxicity.
In an email, Zuber wrote that Vakoc’s CRISPR system will allow systematic CRISPR screens that point toward domains and identify structures for drug development.
Vakoc lives on campus at CSHL with his wife Camila Dos Santos, who studies epigenetic changes that occur after pregnancy. The couple is collaborating in their research. “CRISPR technology is useful for all biologists and my wife is no exception,” he said.
As for his own work, Vakoc expressed an appreciation for the scientific tools bacteria are providing.“Biologists have always been learning from naturally occurring mechanisms used by various organisms” and using them to approach a range of challenges, Vakoc explained.