Increasing fruits and vegetables may protect kidneys
By David Dunaief, M.D.

Chronic kidney disease is on the rise in this country. Approximately 37 million U.S. adults have chronic kidney disease (CKD), with as many as 9 in 10 not aware they have it, according to the Centers for Disease Control and Prevention (CDC) (1). In this article, we will look beyond the more obvious causes of chronic kidney disease, like diabetes, smoking, aging, obesity and high blood pressure (2).
Why is early-stage CKD so important? It is associated with a 40 percent increased risk of developing cardiovascular events, such as heart attacks (3). It also significantly increases the risk of peripheral artery disease (PAD). Those with decreased kidney function have a 24 percent prevalence of PAD, compared to 3.7 percent in those with normal kidney function (4). Of course, it can lead ultimately to end-stage renal (kidney) disease, requiring dialysis and potentially a kidney transplant.
One of the problems with early-stage CKD is that it tends to be asymptomatic. However, there are simple tests, such as a basic metabolic panel and a urinalysis, that will indicate whether a patient may have mild chronic kidney disease. These indices for kidney function include an estimated glomerular filtration rate (eGFR), creatinine level and protein in the urine. While the other two indices have varying ranges depending on the laboratory used, a patient with an eGFR of 30 to 59 mL/minute/1.73 m2 is considered to have mild disease. The eGFR and the kidney function are inversely related, meaning as eGFR declines, the more severe the chronic kidney disease.
What can be done to stem early-stage CKD, before complications occur? There are several studies that have looked at medications and lifestyle modifications and their impacts on its prevention, treatment and reversal. Let’s look at the evidence.
Leveraging Medications
Allopurinol is usually thought of as a medication to prevent gout. However, in a randomized controlled trial, with 113 patients, results show that allopurinol may help to slow the progression of CKD, defined in this study as an eGFR less than 60 mL/min/1.73 m2 (5). The group using 100 mg of allopurinol showed significant improvement in eGFR levels (compared to the control group over a two-year period. The researchers concluded that allopurinol slowed CKD progression. Allopurinol also decreased cardiovascular risk by 71 percent.
Fibrates are a class of drug usually used to boost HDL (“good”) cholesterol levels and reduce triglyceride levels, another cholesterol marker. Fibrates have gotten negative press for not showing improvement in cardiovascular outcomes. However, in patients with mild to moderate CKD, a meta-analysis (a group of 10 studies) showed a 30 percent reduction in major cardiovascular events and a 40 percent reduction in the risk of cardiovascular mortality with the use of fibrates (6). This is important, since patients with CKD are mostly likely to die of cardiovascular disease.
The authors concluded that fibrates seem to have a much more powerful beneficial effect in CKD patients, as opposed to the general population. So, there may be a role for fibrates after all.
Diet’s impact
Fruits and vegetables may play a role in helping patients with CKD. In one study, the results showed that fruits and vegetables work as well as sodium bicarbonate in improving kidney function by reducing metabolic acidosis levels (7).
What is the significance of metabolic acidosis? It means that body fluids become acidic, and it is associated with chronic kidney disease. The authors concluded that both sodium bicarbonate and a diet including fruits and vegetables were renoprotective, helping to protect the kidneys from further damage in patients with CKD. Alkali diets are primarily plant-based, although not necessarily vegetarian or vegan diets. Animal products tend to cause an acidic environment. The study was one year in duration with 77 patients.
In the Nurses’ Health Study, results show that animal fat, red meat and sodium all negatively impact kidney function (8). The risk of protein in the urine, a potential indicator of CKD, increased by 72 percent in those participants who consumed the highest amounts of animal fat compared to the lowest, and by 51 percent in those who ate red meat at least twice a week. With higher amounts of sodium, there was a 52 percent increased risk of having lower levels of eGFR.
The most interesting part with sodium was that the difference between higher mean consumption and the lower mean consumption was not that large, 2.4 grams compared to 1.7 grams. In other words, the difference between approximately a teaspoon of sodium and three quarters of a teaspoon was responsible for the decrease in kidney function.
In my practice, when CKD patients follow a vegetable-rich, nutrient-dense diet, there are substantial improvements in kidney functioning. For instance, for one patient, his baseline eGFR was 54 mL/min/1.73 m2. After one month of lifestyle modifications, his eGFR improved by 9 points to 63 mL/min/1.73 m2, which is a return to “normal” functioning of the kidney. Note that this is an anecdotal story and not a study.
Therefore, it is important to have your kidney function checked with mainstream tests. If the levels are low, you should address the issue through medications and/or lifestyle modifications to manage and reverse early-stage CKD. Don’t wait until symptoms and complications occur. In my experience, it is much easier to treat and reverse a disease in its earlier stages, and CKD is no exception.
References:
(1) CDC.gov. (2) JAMA. 2004;291:844-850. (3) N Engl J Med. 2004;351:1296-1305. (4) Circulation. 2004;109:320–323. (5) Clin J Am Soc Nephrol. 2010 Aug;5:1388-1393. (6) J Am Coll Cardiol. 2012 Nov. 13;60:2061-2071. (7) Clin J Am Soc Nephrol. 2013;8:371-381. (8) Clin J Am Soc Nephrol. 2010; 5:836-843.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com.










 “We are pleased to be able to offer a large, safe vaccination site at the Town’s Senior Center, something we have been working on with the Governor’s office for some time now,” said Supervisor Chad A. Lupinacci. “We look forward to the day we can reopen this community facility to our senior residents and end the isolation many continue experiencing for over a year now: these vaccinations are getting us one step closer to normal.”
“We are pleased to be able to offer a large, safe vaccination site at the Town’s Senior Center, something we have been working on with the Governor’s office for some time now,” said Supervisor Chad A. Lupinacci. “We look forward to the day we can reopen this community facility to our senior residents and end the isolation many continue experiencing for over a year now: these vaccinations are getting us one step closer to normal.” 



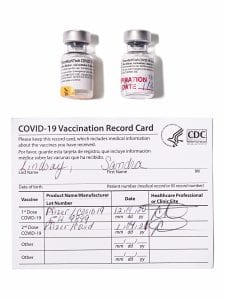 “December 14 was a historic moment for all: the day the very first COVID-19 vaccine was administered in the United States,” said
“December 14 was a historic moment for all: the day the very first COVID-19 vaccine was administered in the United States,” said 


 Our waste stream includes packaging materials and paper goods. Bill S1185 has been introduced by Senator Todd Kaminski and it will be followed by A5801, to be introduced by Assemblyman Steve Englebright. They require producers and manufacturers to finance the recycling of their packaging materials and plastics, with incentives for finding ways of making recycling easier. Within three years of the bill’s implementation, producers will have to comply with the provisions of the bill or work with a producer responsibility organization.
Our waste stream includes packaging materials and paper goods. Bill S1185 has been introduced by Senator Todd Kaminski and it will be followed by A5801, to be introduced by Assemblyman Steve Englebright. They require producers and manufacturers to finance the recycling of their packaging materials and plastics, with incentives for finding ways of making recycling easier. Within three years of the bill’s implementation, producers will have to comply with the provisions of the bill or work with a producer responsibility organization.


