With a dramatic thumbs down gesture from U.S. Sen. John McCain (R-Arizona) in the middle of the night July 28, the GOP-backed health care bill was effectively killed in the United States Senate, leaving the future of health care in the country, state and county a mystery.
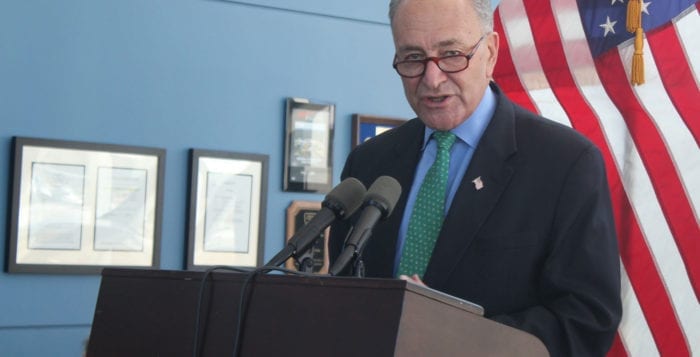
“First: I want to thank Sens. [Lisa Murkowski (R-Alaska)], [Susan Collins (R-Maine)], and McCain for showing such courage, strength, and principle.”
— Chuck Schumer
As a result of the vote, the Affordable Care Act, or Obamacare, remains the law of the land for the time being, despite rhetoric from President Donald Trump (R) suggesting the system is on the verge of collapse. In New York, a universal health care bill progressed past the state assembly and has been in committee since June 2016, awaiting state senate approval and a final signature from Gov. Andrew Cuomo (D). A New York State health care bill would supersede federal law.
“First: I want to thank Sens. [Lisa Murkowski (R-Alaska)], [Susan Collins (R-Maine)], and McCain for showing such courage, strength, and principle,” U.S. Sen. and Senate Minority Leader Chuck Schumer (D-New York) said on Twitter July 28. The three Republican senators voted in line with the 48 Democrats to effectively kill the bill, despite the GOP majority. “To everyone who called, tweeted, emailed, and raised their voice in any way: thank you. Your stories matter. But we are not celebrating. We are relieved — for the millions of Americans who can keep their insurance and breathe a little easier. Now, it’s time for the Senate to come together in a bipartisan way to fix the problems that exist in our health care system. We can stabilize the markets through funding cost sharing reduction and creating reinsurance programs, which keep premiums, deductibles down.”
U.S. Rep. for New York’s 3rd Congressional District Tom Suozzi (D-Glen Cove) released a proposal July 31 with the Problem Solvers Caucus, a bipartisan group of legislators which Suozzi serves as the vice-chair of, that would “stabilize the individual insurance market,” in the wake of the vote, according to a press release. The plan would create a dedicated stability fund to reduce premiums and limit losses of coverage, repeal the 2.3 percent medical device sales tax that is on all medical device supplies, provide clear guidelines for states that want to enter into regional control of their health care and create more options for customers, and more.
“Americans are desperate for Democrats and Republicans to work together to try and tackle the challenges our country faces,” Suozzi said in a statement. “The Problem Solvers Caucus, by proposing this major bipartisan first step, is like an oasis in a desert of dysfunction. We still have much more to do with health care and other issues and we hope our colleagues will join our efforts in this spirit of goodwill and compromise for the common good.”
“The Problem Solvers Caucus, by proposing this major bipartisan first step, is like an oasis in a desert of dysfunction.”
— Tom Suozzi
The New York State Assembly bill for the 2017-18 session, which is currently in committee, would establish The New York Health Act, to create a single-payer health care system.
A single-payer system requires a single-payer fund, which all New Yorkers would pay into to cover health care costs of an individual, instead of through private insurers. In a single-payer system every citizen is covered, patients have the freedom to choose their own doctors and hospitals, and employers would no longer be responsible for health care costs. Suozzi attended a March rally in Huntington in support of a single-payer system for New York.
The U.S. Senate version of the health care bill passed by the House of Representatives in May would have resulted in drastic cuts to Medicaid funding for New Yorkers. According to the Kaiser Family Foundation, a nonprofit organization established to deliver health policy analysis to the public, nearly $92 billion in funding would be cut from New York’s Medicaid expansion dollars between 2020 and 2026.
The predominantly Republican support for the repeal of Obamacare stems from expensive premiums and an individual mandate requiring the purchase of health insurance for all Americans with a fine for noncompliance.
The U.S. Congressional Budget Office was no more optimistic about the GOP health care bill than the Kaiser Family Foundation. A July 20 report from the CBO on one of the many versions of the now-failed senate bill predicted 17 million Americans would be uninsured by 2018 had the bill passed, in addition to increases in premiums.