Early treatment is crucial
By David Dunaief, M.D.

Ah, summer is upon us. Unfortunately, this means that tick season is getting into full swing. Projections for this year’s tick population are ominous, because of seemingly unrelated issues like an increase in last year’s acorn population, which feeds mice that are carriers, and a relatively mild winter (1).
Thus, it is good timing to talk about Borrelia burgdorferi, better known as the bacteria that causes Lyme disease. This bacteria is from the spirochete class and is typically found in the deer tick, also known as the blacklegged tick.
What do deer ticks look like? They are small and can be as tiny as a pencil tip or the size of a period at the end of a sentence. The CDC.gov site is a great resource for tick images and other information related to Lyme disease.
What if you have been bitten by a tick? The first thing you should do is remove it with forceps, tweezers or protected fingers (paper) as close to the skin as possible and pull slow and steady straight up. Do not crush or squeeze the tick, for doing so may spread infectious disease (2). In the study, petroleum jelly, fingernail polish, a hot kitchen match and 70 percent isopropyl alcohol all failed to properly remove a tick. The National Institutes of Health recommend not removing a tick with oil (3).

as seen on the left.
When a tick is removed within 36 to 48 hours, the risk of infection is quite low, according to the Centers for Disease Control and Prevention (4). However, a patient can be given a prophylactic dose of the antibiotic doxycycline, one dose of 200 mg, if the erythema migrans, or bulls-eye rash — a red outer ring and red spot in the center — has not occurred, and it is within 72 hours of tick removal (5). Those who took doxycycline had significantly lower risk of developing the bulls-eye rash and thus Lyme disease; however, treatment with doxycycline did have higher incidence of nausea and vomiting than placebo.
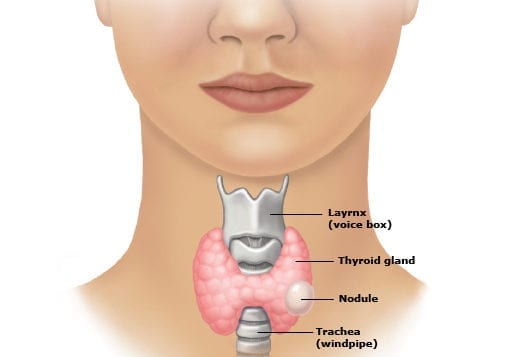
What are the signs and symptoms of Lyme disease? There are three stages of Lyme disease: early stage, where the bacteria are localized; early disseminated disease, where the bacteria have spread throughout the body; and late-stage disseminated disease. Symptoms for early localized stage and early disseminated disease include the bulls-eye rash, which occurs in about 80 percent of patients, with or without systemic symptoms of fatigue (54 percent), muscle pain and joint pain (44 percent), headache (42 percent), neck stiffness (35 percent), swollen glands (23 percent) and fever (16 percent) (6).
Early disseminated disease may cause neurological symptoms such as meningitis, cranial neuropathy (Bell’s palsy) and motor or sensory radiculoneuropathy (nerve roots of spinal cord). Late disseminated disease can cause Lyme arthritis (inflammation in the joints), heart problems, facial paralysis, impaired memory, numbness, pain and decreased concentration (3).
How do we prevent this disease? According to the CDC, we should wear protective clothing, spray ourselves with insect repellent that includes at least 20 percent DEET and treat our yards (4). Always check your skin and hair for ticks after walking through a woody or tall grassy area. Many of us on Long Island have ticks in the yard, so remember to check your pets; even if treated, they can carry ticks into the house. My Golden Retriever, Buddy, whom I loved dearly, died of Lyme complications.
Diagnosis of Lyme disease
Many times Lyme disease can be diagnosed within the clinical setting. When it comes to serologic or blood tests, the CDC recommends an ELISA test followed by a confirmatory Western blot test (4). However, testing immediately after being bitten by a tick is not useful, since the test will tend to be negative, regardless of infection or not (7). It takes about one to two weeks for IgM antibodies to appear and two to six weeks for IgG antibodies (8). These antibodies sometimes remain elevated even after successful treatment with antibiotics.
The cardiac impact
What are some of the complications of Lyme disease? Lyme carditis is a rare complication affecting 1.1 percent of those with disseminated disease, but it can result in sudden cardiac death due to second- or third-degree atrioventricular (AV) node conduction (electrical) block. Among the 1.1 percent who had Lyme carditis, there were five sudden deaths (9). If there are symptoms of chest pain, palpitations, light-headedness, shortness of breath or fainting, then clinicians should suspect Lyme carditis.
Does chronic Lyme disease exist?
There has been a debate about whether there is something called “chronic Lyme” disease. The research, unfortunately, has not shown consistent results that indicate that it exists. In the most recent report, chronic Lyme is refuted (10). In the analysis, the authors comment that the definition of chronic Lyme disease is obfuscated and that extended durations of antibiotics do not prevent or alleviate post-Lyme syndromes, according to several prospective trials. The authors do admit that there are prolonged neurologic symptoms in a subset population that may be debilitating even after the treatment of Lyme disease. These authors also suggest that there may be post-Lyme disease syndromes with joint pain, muscle pain, neck and back pain, fatigue and cognitive impairment.
A previous analysis suggested that chronic Lyme may indeed exist and that post-Lyme disease syndrome is a nebulous term (11). The authors point to several randomized controlled trials (RCT) to help validate their point (12). They believe that the bacteria may be able to evade shorter courses of antibiotics.
Ultimately, it comes down to the IDSA (Infectious Diseases Society of America) arguing against chronic Lyme but in favor of post-Lyme disease syndromes, while the ILADS (International Lyme and Associated Diseases Society) believes chronic Lyme exists.
Regardless, the lingering effects of Lyme can be debilitating. This may be as a result of systemic inflammation (13). Systemic inflammation and its symptoms can be improved significantly with dietary and other lifestyle modifications.
But to throw one more wrench in the mix, the CDC recommends that physicians look beyond Lyme for other possible diagnoses before diagnosing someone with chronic Lyme disease (14).
So what have we learned? Prevention is key to helping stem Lyme disease. If this is not possible, treating prophylactically when pulling off a tick is an important step. Contact your physician as soon as you notice a tick. If you have a bulls-eye rash and it is early, then treatment for two to three weeks needs to be started right away. If it is prolonged and disseminated, then treatment should be for approximately three to four weeks with antibiotics. If it has affected the central nervous system, then IV antibiotics could be needed. Post-Lyme syndrome vs. chronic Lyme disease needs to be discussed with your physician. Symptoms attributed to chronic Lyme could have another cause.
References: (1) npr.org online March 6, 2017. (2) Pediatrics. 1985;75(6):997. (3) nlm.nih.gov. (4) cdc.gov. (5) N Engl J Med. 2001;345(2):79. (6) N Engl J Med. 2003;348(24):2472. (7) Clin Infect Dis. 2008;47(2):188. (8) uptodate.com. (9) MMWR. 2014;63(43):982-983. (10) Expert Rev Anti Infect Ther. 2011;9(7):787-797. (11) Future Microbiol. 2008;3(6):621-624. (12) Neurology 70,992-1003 (2008). (13) J Infect Dis. 2009;199(9:1379-1388). (14) JAMA Intern Med. online Nov. 3, 2014.
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.