COVID-19, which was considered especially threatening to the elderly and those with underlying medical conditions, may also have triggered an inflammatory illness that is sickening children in several places throughout the world, including in Suffolk County.
An inflammatory illness in children with symptoms that mimic Kawasaki disease has sickened seven in Suffolk County and officials are expecting more cases of the rare condition here and throughout the country.
Stony Brook Pediatric Hospital has admitted two cases of the multi-inflammatory pediatric condition, for residents who are 10 and 19 years old.
With other hospitals showing rare but similar unusual pediatric cases, including in the United Kingdom and New York City, the U.S. Centers for Disease Control and Prevention is preparing to release an alert about the inflammatory condition, a CDC spokesman told CNN.
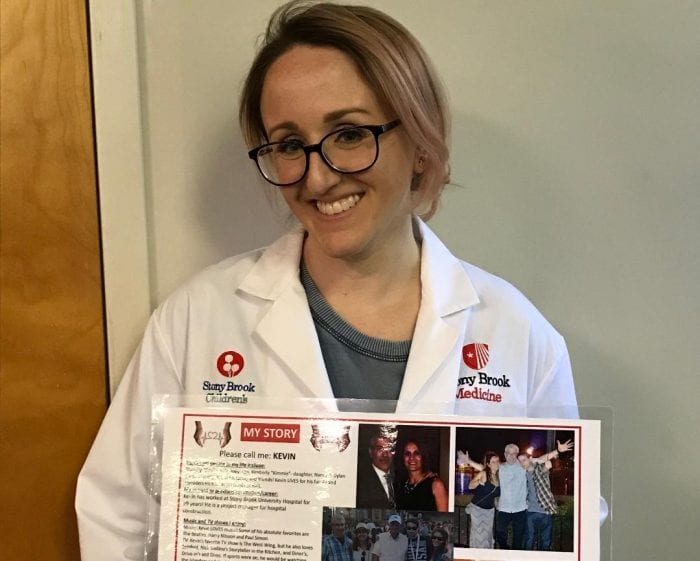
Stony Brook, Pediatric Hospital has been “treating patients like we would treat and approach Kawasaki Disease,” said Christy Beneri, the Fellowship Program Director in Pediatric Infectious Diseases at Stony Brook Children’s Hospital. The hospital has provided intravenous immunoglobulin, a high dose of aspirin and steroids to decrease inflammation and other medications to help suppress the inflammatory syndrome.
This rare inflammatory process in children has developed weeks after a likely mild or asymptomatic case of COVID-19 in mostly healthy younger patients.
Patients can develop symptoms from “days to weeks” after an infection with the virus that has caused the pandemic, Beneri said. The majority of people with this inflammatory reaction are either testing positive for COVID-19 when they come to the hospital or have a positive antibody test, which indicates their immune systems mounted a defense against the virus, Beneri added.
It is unclear to doctors what is causing the progression from a manageable response to the virus to an inflammation that may require a trip to the hospital and to the Intensive Care Unit.
“We are trying to understand how the coronavirus is causing vasculitis,” Beneri said. “It has something to do with how the virus is affecting blood vessels and organs.”
To be sure, Beneri reassured children and their parents that most of the children who are infected with Covid-19 will not develop these inflammatory symptoms later.
“The majority will do well,” Beneri said.
Nonetheless, Beneri anticipated that more pediatric residents in Suffolk County would likely show signs of this inflammatory response.
“If their child is having fever for a number of days, significant vomiting or diarrhea, belly pain, red eyes or a rash, it is important that they speak with their doctor,” Beneri said.
One of the reasons Suffolk County is seeing some cases of this Kawasaki-like response in children now, weeks after the pandemic infected thousands in the area, likely relates to the timing of the peak infections, which occurred in the middle of April.
Based on conversations Beneri has had with other pediatricians who are treating patients with similar symptoms, she said the patients tend to be “healthy kids” who have often had a contact with someone in their house who was recently diagnosed with COVID-19.
The child may have brought the virus into the home and passed it along to a parent, who became sick. The child, however, later develops these multiple-symptom inflammatory issues.
While some children have died from this condition, Beneri said the majority of them are recovering.
The duration of hospital stays has varied, with some patients requiring 10 days in the hospital, while others have recovered within a few days. Beneri said Stony Brook has already sent one patient home.
Beneri added Nassau County has also had several teenage patients come in with the same symptoms. She expects more Suffolk pediatric patients with similar symptoms to come to county hospitals.