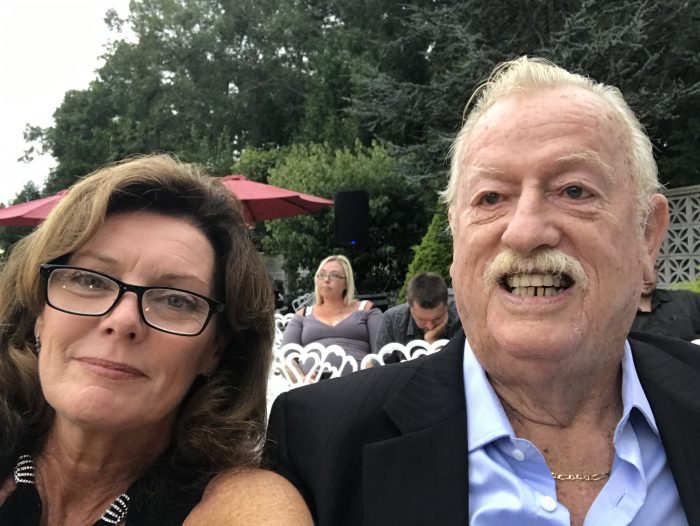
Over 30 years as a plumber took its toll on Daniel Tuttle.

The 79-year old Northport resident felt daily pain in his lower back, which limited his ability to walk for any length of time.
“I always lifted up [stuff] you shouldn’t lift,” Tuttle said. “It was too heavy. Over the years, I got more and more pain.”
Tuttle visited several specialists. His cardiologist recommended he see Dr. Frank Ocasio, director of Acute Pain Management and chair of Pain Management at Huntington Hospital and the director of North Shore Head and Spine in Huntington.
Ocasio recently started performing a therapeutic treatment called Intracept, which involves cutting a small incision in the back, inserting a tube and providing enough heat to deactivate the nerve that causes chronic lower back pain.
About a month after the procedure, Tuttle is pleased to report that his pain has declined from “an 11” to closer to a three on a daily basis.
Several doctors around Long Island have provided the Intracept procedure, which was developed by Relievant Medsystems, over the last few years, including at Stony Brook University and Port Jefferson’s St. Charles Hospital.
Dr. Jonathan Raanan, assistant professor of Neurosurgery, Physical Medicine & Rehabilitation in the Department of Neurosurgery at the Renaissance School of Medicine at Stony Brook University, has performed about 10 such surgeries over the last few years.
Raanan described such lower back pain that lasts more than six months or a year as being something of a “big black hole” in terms of treatment.
In a magnetic resonance image, the disc becomes darker, indicating it doesn’t have good hydration and that it isn’t an effective shock absorber.
Intracept can help reduce the pain.
“It’s very satisfying when someone comes in who has tried everything but the kitchen sink to treat this” who then says “I do feel better,” Raanan said.
Tuttle’s wife Susan, who has been married to him for over three decades, said the procedure has improved his quality of life.
Susan Tuttle said her husband has been able to “do everything he wanted to do.”
Ocasio found the idea of Intracept appealing, particularly because it was a one-time effort that didn’t require ongoing follow up visits.
“There’s not much out there in the pain management space that’s a non medication, a non-opioid strategy that’s a one and done,” Ocasio said.
The surgery is an outpatient procedure and can take anywhere from 45 minutes to two hours, depending on the area over which the nerve is sending a repeated pain signal.
Patients either receive mild sedation or are under general anesthesia.
“People see results within weeks,” Ocasio said. In some cases, they can get relief within 24 hours.

To be sure, the procedure, as with any, involves some level of risk and isn’t appropriate for everyone.
Raanan advised potential patients to discuss the risks and benefits with any provider.
Starting in January, Intracept will have a Current Procedural Terminology, or CPT, code, which will give health care providers a standard way to describe the procedure and insurance companies a way of determining patient eligibility.
Until then, patients need to appeal to indicate to insurance companies what other treatments they’ve had for back pain.
In Raanan’s experience, patients sometimes have flare-ups of other pain that is similar to sciatic discomfort after the treatment for days or even weeks after Intracept.
“That might be a reasonable trade-off in the eyes of the patient,” Raanan added.
Deadening the nerve doesn’t cause any loss of control of motor function, Ocasio said, as the nerve provides a sensory benefit while others provide necessary muscle control.
“You still have multiple nerves around that area,” Ocasio added.
Candidates for this procedure typically have lower back pain associated with activities that require bending forward, like loading a dishwasher or flexing at the waist, Ocasio described.
Ocasio said doctors who perform Intracept receive training under guidance from the company.
Patients interested in this approach are anywhere from their 30s through their late 70s, local doctors said.
For Daniel Tuttle, the procedure provided relief.
“He’s outside, puttering around, doing the things that make him happy,” Susan
Tuttle said.
“It gave me my lifestyle back,” Daniel Tuttle said.
The Tuttles are planning a trip to Italy next summer.
Raanan cautioned that, for at least one patient, the relief led to another problem.
A female patient returned to working out in the gym, where she exercised so vigorously that she created a different spine injury that he treated.
“When patients feel better, they have to remember they are still vulnerable,” Raanan said. “Poor mechanics, postures, flexibility or excessive and prolonged activity come with some risk.”