By Daniel Dunaief
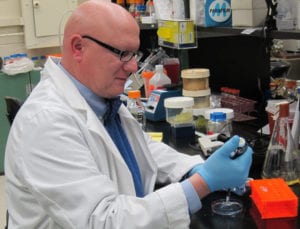
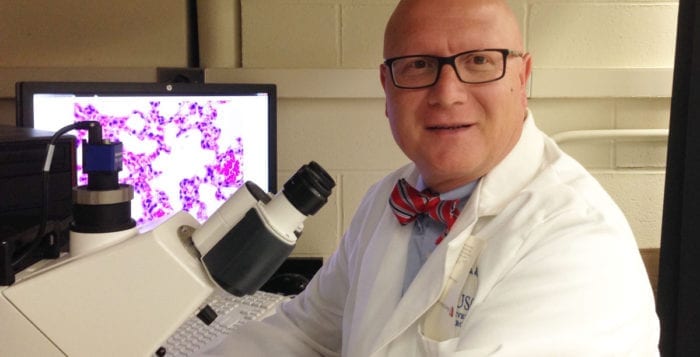
Maurizio Del Poeta is taking another approach to battling fungal infections that can be deadly, particularly for people who are immunocompromised.

A Distinguished Professor at Stony Brook University in the Department of Microbiology and Immunology at the Renaissance School of Medicine at Stony Brook University, Del Poeta has made progress in animal models of various fungal infections in working on treatments and vaccines.
After receiving an additional $3.8 million from the National Institutes of Health for five years, Del Poeta is expanding on some findings that may lead to a greater understanding of the mechanism that makes some fungal infections problematic.
The Stony Brook Distinguished Professor is studying “what makes people susceptible to fungal infections,” he said. “It’s something I’m really passionate about.”
Del Poeta explained that researchers and medical professionals often focus on the people who get sick. Understanding those people who are not developing an infection or battling against a fungus can provide insights into ways to understand what makes one population vulnerable or susceptible and another more resistant.
Expanding such an approach outside the realm of fungal infections could also provide key insights for a range of infections in the future.
Indeed, the awareness of specific signals for other infections could help protect specific populations, beyond those who had general categories like underlying medical conditions, who might be more vulnerable amid any kind of outbreak.
“It’s possible that the study we are doing now with fungi could stimulate interest” in other areas of infectious disease, Del Poeta said.
He suggested that this was “pioneering work” in terms of fungal infections. At this point, his lab has produced “strong preliminary data.”
An important drug treatment side effect as a signal
This investigation arises out of work Del Poeta had done to understand why some people with multiple sclerosis who took a specific drug, called fingolimid, developed fungal infections during their drug treatment.
Del Poeta observed that the drug inhibits a type of immunity that involves the movement of lymphocytes from organs into the bloodstream.
Fingolimid mimics a natural lipid, called a sphingolipid. Del Poeta showed that this sphingolipid is important to contain the fungus Cryptococcus neoformans in the lung. When its level decreases, the fungus can move from the lung to the brain.
Indeed, Fingolimid mimics sphingosin-1-phosphate (S1P) and binds to several S1P receptors.
Del Poeta believes that the pathway between S1P and its receptor regulates the immunity against Cryptococcus. Blocking a specific receptor is detrimental for the host and may lead to reactivation of the fungus.
Putting a team together

Del Poeta has been working with Iwao Ojima, a Distinguished Professor and the Director of the Institute of Chemical Biology and Drug Discovery in the Department of Chemistry at Stony Brook, to create compounds that energize, instead of block, the target of fingolimid.
Del Poeta has recruited two scientists to join his lab in this effort, each of whom has educational experience in nursing.
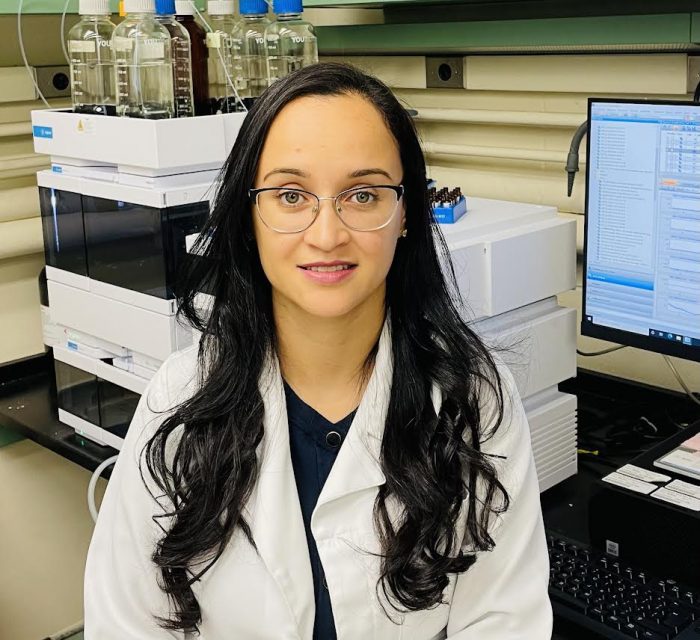
Nathália Fidelis Vieira de Sá, who is a registered nurse at the Federal University of Minas Gerais and a chemistry technician at Funec- Contagem City, will join the lab as a technician in the second week of September.
Fidelis Vieira de Sá, who currently lives in her native Brazil, is an “expert on collecting and analyzing organs for mice,” explained Del Poeta in an email.
For her part, Fidelis Vieira de Sá is thrilled to join Del Poeta’s lab at Stony Brook. “I’m very excited,” she said in an email. She is eager to get started because the research is “of such great relevance to public health” and is occurring at such a “renowned institution.”
Fidelis Vieira de Sá believes this is a public health issue that could have a positive impact on people with immunodeficiency conditions who need effective treatment so they live a better, longer life. When she was a peritoneal dialysis nurse, she had a few patients who had fungal infections.
“This is very serious and challenging, detection is difficult, and the life expectancy of these patients drops dramatically with each episode of infection,” she explained.
Fidelis Vieira de Sá, who has never lived outside Brazil, is eager for new experiences, including visiting Central Park, the Statue of Liberty, Times Square, and the One World Trade Center Memorial.
As for the work, she hopes that, in the near future, Del Poeta will “be able to explain this mechanism deeply and to develop new drugs that will act on this receptor.”

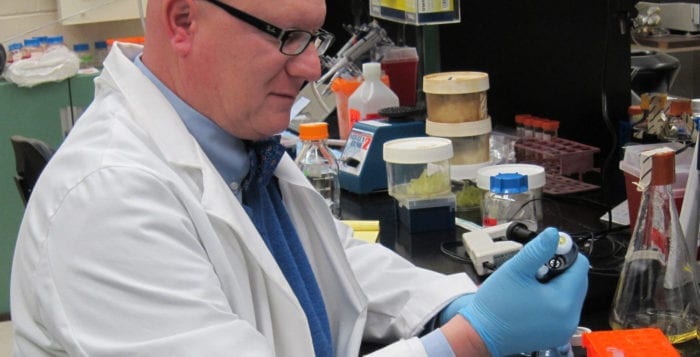
Dr. Marinaldo Pacífico Cavalcanti Neto, who is an Assistant Professor at Federal University of Rio de Janeiro, will be arriving at Stony Brook University on August 6. Dr. Neto earned his bachelor of science in nursing and has a PhD in biochemistry from the Medical School of Ribeirão Preto at the University of São Paulo.
Del Poeta described Dr. Neto as an “expert on animal handling and genotyping,”
Dr. Neto recognizes the burden of fungal infections around the world and hoped to work with someone with Del Poeta’s credentials and experience in immunology and infection.
Understanding how cells eliminate infection, how cells might have a lower capacity to control an infection, and looking for how cells respond to treatments such as fingolimid could be a “great strategy to understand why these are so susceptible,” he said.
While Dr. Neto’s background is in immunology, he hopes to learn more about molecular biology.
Unlike Fidelis Vieira de Sá, Dr. Neto, who will live in Centereach, has worked previously in the United States. He has experience at the National Institutes of Health and at the University of California at San Diego and has been attending Del Poeta’s lab meetings from a distance for about a month.
Dr. Neto, whose interest in science increased while he watched the TV show Beakman’s World while he was growing up, is eager to work in an area where he can apply his research.
He appreciates that his work may one day “be used in the generation of protocols in a clinic.