By Daniel Dunaief
Even as some antibiotics and anti cancer treatments help beat back infections and diseases such as cancer, pathogens and diseases can develop resistance that render these treatments less effective.
Researchers at pharmaceutical companies and universities spend considerable time trying to ensure therapies continue to work. Companies make derivatives of existing drugs or they combine drugs to reduce resistance. They also develop new agents to combat drug-resistant tumors.
Using a chemical process that won his mentor K. Barry Sharpless a Nobel Prize, John Moses, a Professor at Cold Spring Harbor Laboratory, has deployed a new version of click chemistry to assemble biologically active compounds quickly and effectively, which could be used for further development into potential therapies.
Akin to fastening a seatbelt or assembling LEGO blocks, click chemistry benefits from an efficient system to create reliable end products, with the additional advantage of minimizing waste products or impurities.
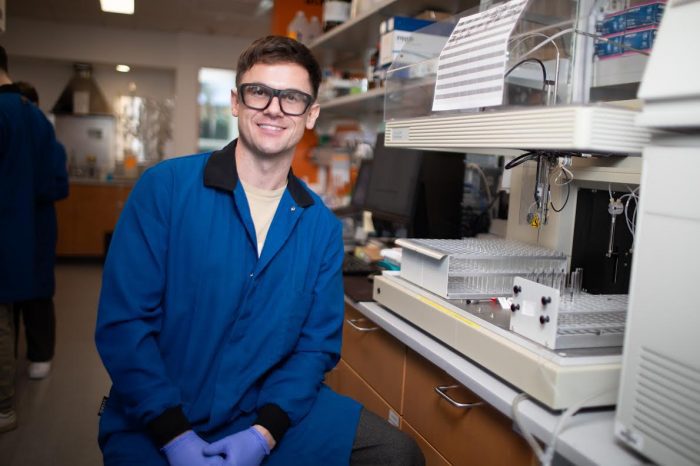
Recently, Research Investigator Joshua Homer, who has been in Moses’s lab for over three years, published a paper in Chemical Science in which he created several libraries of over 150 compounds. He screened these for activity in anticancer or antibiotic assays.
The newer click process, called Accelerated SuFEx Click Chemistry, or ASCC, involves “less synthetic steps,” said Homer. ASCC can use functional groups like alcohols, that are naturally found in numerous commercially available compounds, directly. Homer can and has used commercially available alkyl and aryl alcohols as fragments in this application of ASCC.
This approach “allows us to explore chemical space so much faster,” Homer said.
In an email, Moses suggested that the paper “demonstrates that SuFEx chemistry can be a feasible and speedy approach compared to traditional methods.”
To be sure, the products could still be a long way from concept to bedside benefit.
“It’s important to note that while the chemistry itself shows promise, the actual application in drug development is complex and can take many years,” Moses added.
The research contributed to finding compounds that may be promising in treating various conditions and represent initial findings and potential starting points for further development, Homer added.
Specifically, Homer took inspiration from the structure of combrestastatin A4 when developing microtubule targeting agents.
The chemicals he produced had good activity against drug-resistant cancer cell lines that resist other treatment options.
Homer also modified the structure of dapsone, generating a derivative with greater activity against a strain of M. tuberculosis that is otherwise resistant to dapsone.
“Strains of bacteria develop resistance to antibiotics,” said Homer. Derivatization of antibiotic structures can generate compounds that maintain activity.
Breast cancer
In creating these compounds, Homer bolted on different commercially available fragments and developed potential nano-molar treatments that could be effective against triple-negative breast cancer.
At this point, he has evaluated two lead agents in two dimensional cell culture and against patient-derived organoids. Homer did this work in collaboration with the lab of CSHL Cancer Center director David Tuveson.
Organoids can help gauge the potential response of a patient’s tumor to various treatments.
Homer found that eight of the microtubule targeting agents were more potent than colchicine against HCT-15. This cancer cell line, he explained, is known to have upregulated efflux, which is a major cause of drug resistance in cancer cells.
His compounds maintained a similar potency between two dimensional cell lines and organoids. Often, compounds are less potent in organoids, which makes this a promising discovery.
Making molecules and screening them for function to discover lead candidates is one of the first steps in the drug discovery process, with considerable optimization and regulatory steps necessary to generate a drug for the clinic.
Promising treatments sometimes also cause cellular damage in healthy tissue, which reduces the potential benefit of any new treatment. Effective cancer drugs are selective for cancer cells over normal cells.
At this point, the molecules Homer creates involve a search for function, he said. “Once we identify the reaction, we can remake our molecule to confirm it is our compound that is causing a reaction.”
Click chemistry doesn’t necessarily lead to solutions, but it enables scientists and drug companies to create and test molecules more rapidly and with considerably less financial investment.
Click solutions
Click chemistry has affected the way Homer thinks about problems outside the lab.
“I think more about doing things quickly and how to tackle the issues we face, rather than using brute force in one direction,” he said. “We can go in lots of directions and probe. We should be looking at all sorts of baskets at once to solve the issues we have.”
Originally from Tauranga, New Zealand, Homer enjoys traveling around the country, visiting new cities and interacting with different people. A resident of Huntington, Homer is looking forward to an upcoming visit from his parents Dave and Debbie and his aunt Carol, who are making their first trip to the continental United States.
“One of my favorite things about being a scientist is that I can bring my parents out of their comfort zone,” he said. His parents live on a small lifestyle block with several sheep and chickens.
Moses lauded the contributions Homer has made to the lab, including providing mentorship to other students.
As for click chemistry, Homer appreciates how the reactions create opportunities even for those without advanced backgrounds in chemistry.
Click chemistry creates the opportunity to help non-scientists understand scientific concepts more easily.
“I can give a high school student the reagents and substrates and they can reliably make biologically active anticancer agents or antibiotics,” he said. “That helps connect science and drug discovery with the community.”