SBU’s Pathology team links protein level to pancreatic cancer aggression
By Daniel Dunaief
The prognosis and treatment for cancer varies, depending on the severity, stage and type of disease. With pancreatic ductal adenocarcinoma, the treatment options are often limited and the prognosis for most patients by the time doctors make a diagnosis is often bleak.
Researchers at the Renaissance School of Medicine’s Pathology Department at Stony Brook University have been testing for the presence of a protein called keratin 17, or K17, by staining tissue specimens or needle aspiration biopsy specimens. This measures the proportion of tumor cells that have high levels of expression.
This protein is typically active during embryological development or in stem cells, which are a type of cell that can differentiate into a wide range of other cells. It is also active in pancreatic cancer.
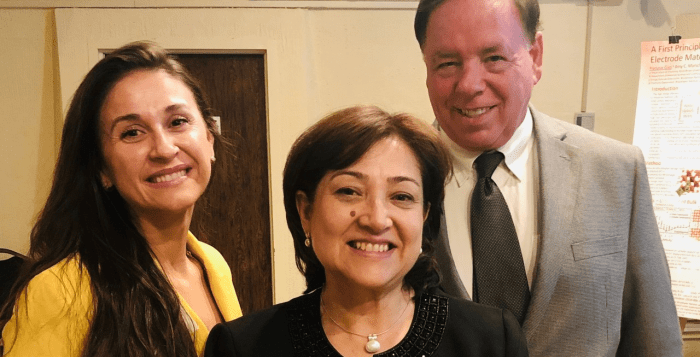
Ken Shroyer, department chairman; Luisa Escobar-Hoyos, assistant professor of pathology; and Lucia Roa, assistant professor of pathology recently published a paper in the journal Scientific Reports in which they documented how the level of this protein can indicate the prognosis for patients. K17 above a certain level typically suggests a worse prognosis.
The Stony Brook scientists want to understand why some pancreatic cancers are more aggressive than others, with the hope that they might be able to develop more effective ways to treat the most aggressive form of the disease.
In the recent research, the level of K17 not only indicated the prognosis for the most aggressive form of the disease, but it is also considered a “cause of making the tumors more aggressive,” Escobar-Hoyos added, which confirmed their previously published research and which unpublished data also supports.
Shroyer suggested that this research paper has been a validation of their plan to pursue the development of K17 as a way to differentiate one form of this insidious cancer from another.
While other cancers, such as cervical cancer, have proven quicker and easier to use K17 for its predictive power, the current work reflects the lab’s focus on pancreatic cancer. As such the research is a “great step forward to generate our first pancreatic cancer paper,” Shroyer said. His lab had previously published papers on other biomarkers in pancreatic cancer.
Escobar-Hoyos indicated that she and Shroyer anticipate that K17, which is one of a family of 54 different types of keratins in the human body, likely plays numerous roles in promoting cancer.
Indeed, K17 may promote the invasiveness of these cells, allowing them to spread from the original organ, in this case the pancreas, to other parts of the body. They are testing that concept through ongoing work in their lab.
The researchers believe that K17 may accelerate metastasis, but that line of thinking is “still at a relatively early stage,” Escobar-Hoyos said.
This protein may also change the metabolism of the cell. They believe K17 blocks the uptake of certain drugs by enhancing specific metabolic pathways.
Additionally, K17 causes the degradation of p27, which is a tumor suppressor that controls cell division.
The researchers used two different ways to monitor the levels of protein, through mRNA analysis and through immunohistochemical localization. In the latter case, that involved staining the cells to look for the presence of the protein.
Roa, who is the first author on the paper, stained the slides and worked with Shroyer to score them.
The assistant professor, who came to Long Island with her daughter Laura who earned her bachelor’s degree and master’s in public policy at SBU, had been a pathologist and medical doctor when she lived in Colombia. She learned the IHC staining technique at Yale University just after she graduated from medical school and worked for six years as a postdoctoral fellow on several projects using IHC.
Roa is thrilled that she’s a part of a supportive team that could help develop techniques to improve patient diagnosis and care.
“We care deeply about developing a tool that will help us to treat patients and we value working together to accomplish this,” Roa explained in an email.
At this point, Shroyer and his team have identified key factors that cause K17 to be overexpressed. They are pursuing this line of research in the lab.
“We think K17 expression is dictated by something different than genetic status,” said Escobar-Hoyos. “This is speculation, but we think it might be triggered based on a patient’s immunity.”
After this study, the pathology team is looking to validate their results through different cohorts of patients. They are working with the Pancreatic Cancer Action Network and their scientific collaborators at Perthera Inc. to process tissue sections from these cases for K17 staining in their lab.
They are also at the early stages in the development of a collaboration with investigators at MD Anderson Cancer Center.
“If we can validate that K17 IHC testing is able to predict a response to the standard of care, then we’ll have permission to start a prospective analysis linked to a clinical trial,” Shroyer said.
Shroyer’s team is trying to understand how K17 becomes activated, what happens when they block that activation, and how it impacts the survival and tumor growth in animal models of pancreatic cancer.
In collaborations with other researchers, they are exploring how K17 impacts the therapeutic vulnerability of pancreatic cancer to over 2,000 FDA-approved compounds.
“There are a discrete list of compounds that are able to kill K17 positive cells,” Shroyer said. He is aiming to start phase 0 trials to validate the molecular model. If the data is sufficiently convincing, they can apply to the FDA to begin phase 1 trials.
He hopes this study is the first of many steps the lab will take in providing clues about how to diagnose and treat pancreatic cancer, which has been an intractable disease for researchers and doctors.
“This paper helps establish and confirm that K17 is an important and promising prognostic biomarker in pancreatic cancer,” Shroyer said. “For us, this is foundational for all the subsequent mechanistic studies that are in progress to understand how K17 drives cancer aggression.”