Medical Compass: Rheumatoid arthritis treatment and its complications
By David Dunaief, M.D.
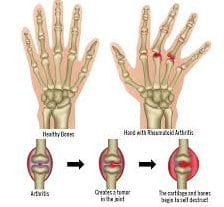
Rheumatoid arthritis (RA) is one of many autoimmune diseases where the body’s immune system begins to attack the body’s own tissue. RA results in systemic (throughout the body) inflammation, which initially affects the synovium (lining) of the small joints in both the hand and the feet bilaterally, as well as the wrists and ankles (1). It causes pain, stiffness and swelling of the joints.
RA, like most autoimmune diseases, affects significantly more women than men and can be incredibly debilitating (2). It affects approximately 1 percent of the U.S. population (3). Fortunately, treatments have helped to significantly improve sufferers’ quality of life.

RA may be treated initially with acetaminophen and NSAIDs (such as ibuprofen), depending on its severity. To help stop progression and preserve the joints, disease-modifying anti-rheumatic drugs (known as DMARDs) may be used. They are considered the gold standard of treatment for RA and include methotrexate, which has been around the longest and is a first-line therapy; plaquenil (hydroxycholorquine); and TNF inhibitors, such as Enbrel (etanercept), Humira (adalimumab) and Remicade (infliximab).
DMARDs work by reducing inflammation and acting as immunosuppressives, basically tamping down or suppressing the immune system. These drugs have helped RA patients improve their quality of life, preserving joint integrity and causing RA to go into remission. The goal of these drugs is to reduce synovitis, or inflammation in the joints, helping to lessen joint damage. They can be quite effective. Unfortunately, compliance can be an issue. In addition, corticosteroids can be used to suppress inflammation.
The yin and yang of medications
In a meta-analysis (a group of 28 studies), the results showed that DMARDs reduced the risk of cardiovascular events by up to 30 percent, while NSAIDs and corticosteroids increased the risk (4). However, oral steroids have been found to increase the risk of heart complications, approximately a 50 percent rise in risk. This may be one reason rheumatologists encourage their RA patients to discontinue oral steroid treatments as quickly as possible.
In an observational study, the results reaffirmed that corticosteroids increased the risk of a heart attack in RA patients, this time by 68 percent (5). The study involved over 8,000 patients with a follow-up of nine years. Interestingly, there was a dose-response curve. In other words, the results also showed that for every 5-mg increase in dosage, there was a corresponding 14 percent increase in heart attack risk.
The downside of using immunosuppressive drugs
Unfortunately, DMARDs have significant adverse effects. In 2011, the FDA found there were 100 cases of Listeria and Legionella pneumonia infections associated with these drugs. Therefore, a black-box warning was placed on all TNF inhibitors cautioning about serious or life-threatening side effects, such as opportunistic infections — more likely in combination with other immunosuppressives — and malignancy. The median duration that patients were on the drugs when they experienced infections was about 10 months. However, most patients were also on methotrexate and steroids at the time of infection.
Anecdotally, I had a patient who had previously developed pneumonia twice, multiple basal-cell carcinomas and one episode of melanoma. These were all attributed to use of a TNF inhibitor.
Skin cancer risk
In 2009, the FDA warned that there is an increased risk of cancer after about 30 months of treatment, especially with TNF inhibitors. A 2011 meta-analysis (a group of 28 studies) found that TNF inhibitors may increase the risk of cancers, including skin cancers (6). In four of the studies, there was a 45 percent elevated risk of developing skin cancer other than melanoma. However, in data pooled from two of the studies, there was a 79 percent greater chance of developing melanoma. All the studies in this analysis were observational studies, and the absolute risk of developing cancer is small. The good news is that this analysis did not appear to show increased risk of lymphoma.
Cardiovascular disease
Patients with RA are at a threefold increased risk of developing coronary artery disease, compared to the general population (7). Those RA patients who stopped taking statins for high cholesterol and/or heart disease had a 60 percent increased risk of cardiovascular mortality and a 79 percent increased risk of all-cause death after three months (8). Though statins have their pitfalls, they can be potentially lifesaving in the right context. Don’t discontinue statins before consulting your physician.
Additional complications from RA
RA can also affect organs and the surrounding tissue. Thus, complications from RA include heart disease, stroke, atrial fibrillation, chronic obstructive pulmonary disease, fracture risk, as well as uveitis and scleritis (inflammatory disorders of the eye).
Nonpharmacologic approaches
Exercise and fish oil have shown reductions in symptomatology and joint inflammation. In a meta-analysis (a group of 17 trials), omega-3 fish oil reduced joint pain intensity, as reported by patients, minutes of morning stiffness, number of painful joints and NSAID use significantly (9). The dose was at least 2.7 g of EPA plus DHA in the omega-3 fish oil and took at least 12 weeks of treatment to see a benefit. Exercise is also important to relieve joint pain and stiffness. In a meta-analysis of 14 studies, there was a 69 percent reduction in pain with aerobic exercise (10). Understandably, however, a study found that 42 percent of RA patients don’t work out at the recommended minimum of 10 minutes of moderate exercise daily (11). The reasons were that half were either not motivated or believed that exercise had no benefit.
Prevention
In the Iowa Women’s Health Study, results showed that supplemental vitamin D decreased the risk of RA by 34 percent (12). This study involved almost 30,000 women followed over an 11-year period.
The best way to treat an autoimmune disease like rheumatoid arthritis is to prevent it with an anti-inflammatory diet, exercise and omega-3 fish oil. Barring that, however, it is encouraging that DMARD treatments may be effective at half the dose once the disease has been suppressed significantly. Therefore, a low-dose pharmacological approach coupled with nonpharmacological lifestyle adjustments may produce the best outcomes with the fewest adverse reactions.
References: (1) www.ncbi.nlm.nih.gov. (2) www.mayoclinic.com. (3) Arthritis Rheum. 2008;58:15-25. (4) Ann Rheum Dis 2015;74(3):480-489. (5) Rheumatology 2013;52:68-75. (6) Ann Rheum Dis. 2011 Nov;70(11):1895-1904. (7) Ann Rheum Dis. 2007;66(1):70. (8) Arthritis Care Res [Hoboken]. 2012 Mar 29. (9) Pain. 2007 May;129(1-2):210-223. (10) Br J Sports Med. 2011;45(12):1008-1009. (11) Arthritis Care Res [Hoboken]. 2012 Apr;64(4):488-493. (12) Arthritis Rheum. 2004 Jan;50(1):72-77.
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.