A paper published this week in Immunity, a leading research journal highlighting discoveries in immunology by Cell Press, lays the groundwork to better understand and treat Crohn’s disease, a type of Inflammatory Bowel Disease (IBD). Beneficial interactions among intestinal cell types limit the harmful effects of a dysregulated gut microbiota, which is comprised of trillions of bacteria, viruses, and other microorganisms. These cell-cell interactions are essential to maintain a healthy gut and dysregulation of this cellular “crosstalk” can predispose the development of IBD.

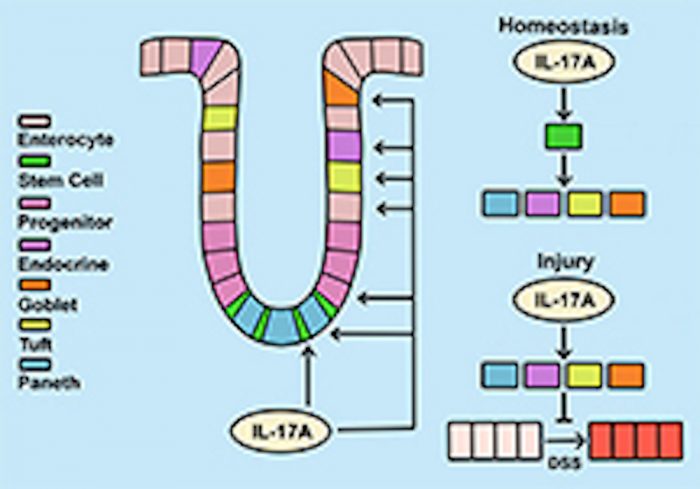
Led by Pawan Kumar, BVSc, PhD, of the Renaissance School of Medicine at Stony Brook University, the research identified a new role for Interleukin-17A (IL-17A), an immune cell-derived cytokine, in promoting selective epithelial cell development as well as limiting inflammation during colitis.Although drugs that target IL-17A are highly effective against psoriasis, an autoimmune condition, the same drugs result in adverse effects when used to treat the inflammatory responses of Crohn’s. While targeting IL-17A may reduce the pathogenesis of certain inflammatory responses, it is unclear why these treatments had opposing effects in Crohn’s patients. The research team has addressed this underlying question.
“We identified a new role for IL-17A in the intestinal inflammatory process by regulating a type of stem cell (Lgr5+) and progenitor cell function,” said Kumar, Senior Author and an Assistant Professor in the Department of Microbiology and Immunology. “We found that IL-17A acts on intestinal stem cells to promote secretory cell lineage commitment. In addition, impaired IL-17A signaling to secretory cells (ATOH1+) exacerbates colitis.
”The research team tested their findings in different murine models. Upon collaborating with Ken Cadwell of New York University, they confirmed their results in human organoids. They found that IL-17A stimulated secretory cell differentiation in cystic human intestinal organoids.“Our data suggest that there is a ‘cross talk’ between immune cells and stem cells that regulates secretory cell lineage commitment and the integrity of the mucosa,” summarizes Kumar.
The authors believe their findings will help further research and lay the groundwork for future clinical studies that investigate the therapeutic potential of IL-17A and/or its downstream effector proteins.This research is supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases, the Crohn’s and Colitis Foundation, the SUNY Research Foundation and a National Science Foundation Graduate Research Fellowship.